Payments linked to
higher odds of doctors prescribing certain cancer drugs
UNC Lineberger Comprehensive Cancer
Center
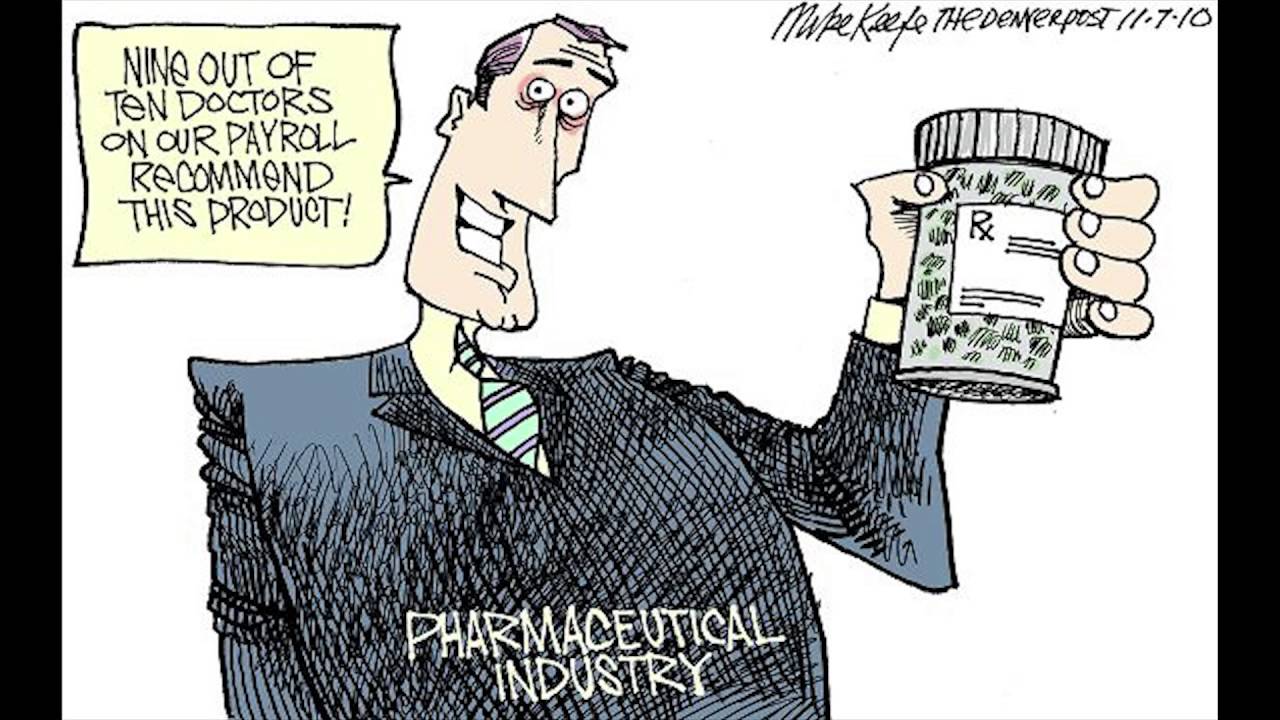 Physicians paid by pharmaceutical
companies for meals, talks and travel had higher odds of prescribing those
companies' drugs to treat two cancer types, a University of North Carolina
Lineberger Comprehensive Cancer Center-led study has found.
Physicians paid by pharmaceutical
companies for meals, talks and travel had higher odds of prescribing those
companies' drugs to treat two cancer types, a University of North Carolina
Lineberger Comprehensive Cancer Center-led study has found.
Researchers show that when
physicians had to choose between multiple, on-patent drugs for metastatic
kidney cancer and chronic myeloid leukemia, they were more likely to prescribe
drugs from companies they had received these "general" payments from.
While they found that these payments
for lodging and meals were linked to higher odds of prescribing certain drugs,
that wasn't consistently the case for payments for research.
"Ideally, therapy choices should be based on two things, and two things only: medical evidence and patient preference," said Aaron Mitchell, MD, a fellow in the UNC School of Medicine Division of Hematology & Oncology and the study's lead author.
"As patient advocates, we
should try to eliminate any barriers to this. We saw a pretty consistent
increase in prescribing of a company's drug stemming from what we call 'general
payments,' which don't go directly for research, but instead are paid to
physicians for consulting, meals, travel and lodging for conferences or talks.
This raises the possibility that drug companies are able to influence
prescribing practices through gifts to physicians."
Last year, several research groups
identified links between pharmaceutical payments and prescription practices.
A 2016 study published in JAMA Internal Medicine determined that doctors who received a single meal promoting a certain brand-name drug prescribed those drugs for depression, high cholesterol and heart disease at higher rates.
Another study in the same journal
last year found a link between industry payments and higher rates of
prescriptions for brand-name cholesterol drugs.
In oncology, the stakes are high,
Mitchell said, since cancer drugs can have significant side effects and
financial costs.
"This pattern is worrisome
since promotional efforts by pharmaceutical companies tend to focus on newer
products, which may steer providers and patients to more expensive
treatments," said the study's senior author Stacie B. Dusetzina, PhD, a
UNC Lineberger member and assistant professor in the UNC Eshelman School of
Pharmacy and Gillings School of Global Public Health. "This could
ultimately drive up costs for patients and taxpayers."
To examine whether company payments
are influencing prescription choice in cancer care, researchers analyzed
prescription patterns for Medicare patients with two cancers where there are
multiple treatment options -- metastatic renal cell cancer, which is a type of
kidney cancer, and chronic myeloid leukemia, a blood cancer.
They used publicly available data
reported through Open Payments, a provision of the federal Patient Protection
and Affordable Care Act that required U.S. drug and device manufacturers to
disclose transfers of financial value greater than $10 to physicians and
teaching hospitals.
"We chose these specific drugs
because they are felt to be equally efficacious based on clinical trials,"
Mitchell said. "However, they do have differences in side effect profiles
that a patient taking one of these drugs would notice and feel."
Compared to physicians who didn't
receive any payments, those who received general payments for meals and lodging
from a drug manufacturer had higher odds of prescribing that company's
particular drug for both metastatic renal cell carcinoma, and for chromic
myeloid leukemia.
For renal cell carcinoma, odds were
78 percent higher, and for chronic myeloid leukemia, odds were 29 percent
higher.
The average amount that physicians
received in general payments was $566 for renal cell carcinoma, and $166 for
chronic myeloid leukemia.
"Even for physicians who
received very small payments, we still saw a change in prescription
rates," Mitchell said. "It looks like this shakes out to be a really
good buy for a drug company."
Meanwhile, they did not find a
consistent relationship for physicians who received payments from
pharmaceutical companies solely for research. This doesn't rule out the
possibility of an association, however, Mitchell said.
He called for more research to
explore the impact of research payments on prescription practices, and to
uncover whether the association they found between general payments and
prescription choice was a cause-and-effect relationship.
"This is a 'proof of principle'
study, showing that there is an association between industry payments and
prescribing in cancer care, and that this may also be present for other
treatment choices where the options are not equivalent," Mitchell said.
"If evidence emerges to show
that drug industry payments are not only associated with changes in physician
practice, but cause these changes, then we need to find some solution to
prevent physician-industry relationships from influencing physicians in such a
manner," he added.