Better
bandage promotes powerful healing
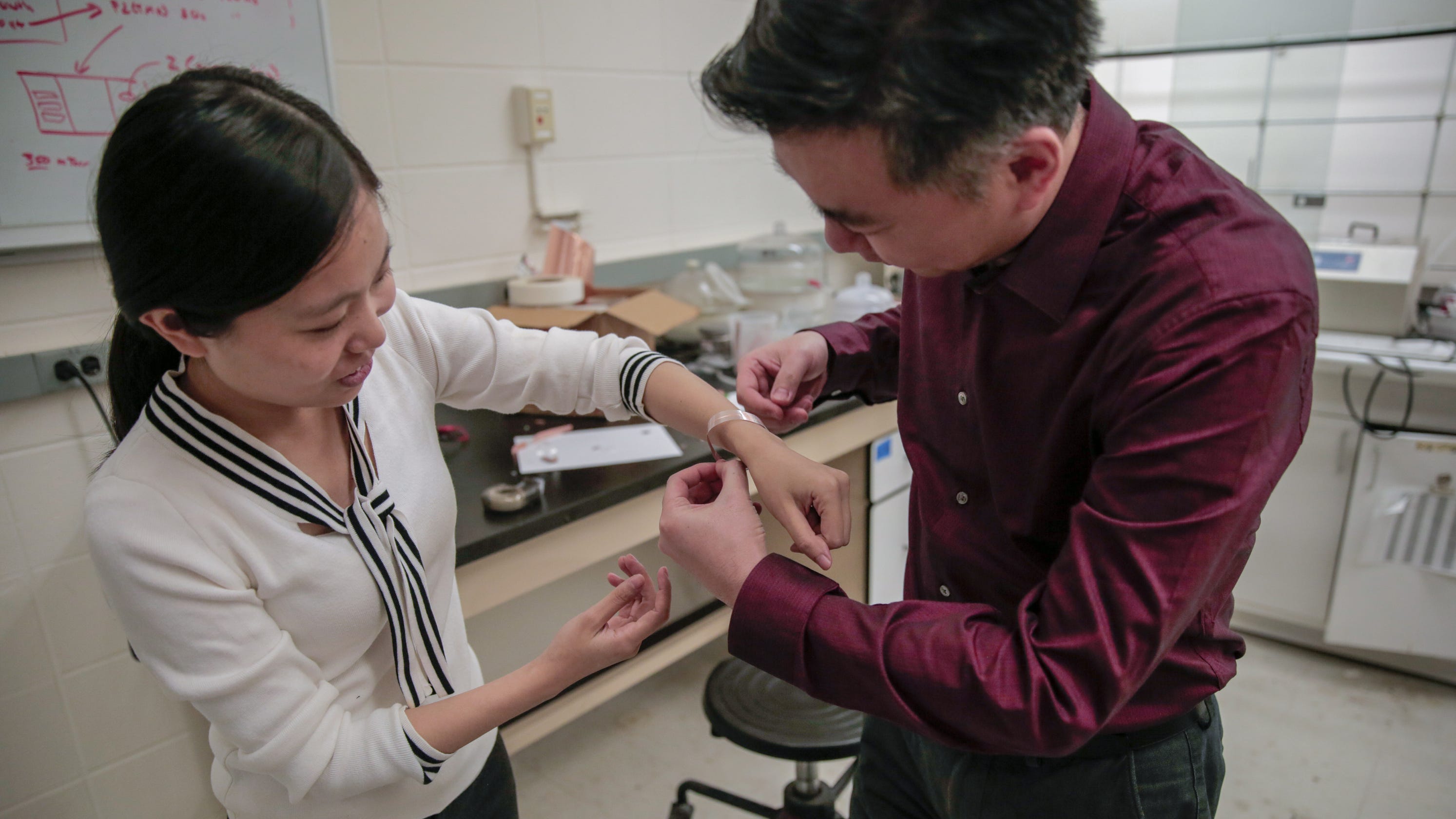
Materials
science and engineering professor Xudon Wang fits a new wound dressing around
the wrist of graduate student Yin Long. The device stimulates healing using
electricity generated from the body’s natural motions. PHOTO BY SAM MILLION-WEAVER
A new, low-cost wound dressing developed by University of Wisconsin–Madison engineers could dramatically speed up healing in a surprising way.
The
method leverages energy generated from a patient’s own body motions to apply
gentle electrical pulses at the site of an injury.
In
rodent tests, the dressings reduced healing times to a mere three days compared
to nearly two weeks for the normal healing process.
“We were surprised to see such a fast recovery rate,” says Xudong Wang, a professor of materials science and engineering at UW–Madison. “We suspected that the devices would produce some effect, but the magnitude was much more than we expected.”
Wang
and collaborators described their wound
dressing method today (Nov. 29, 2018) in the journal ACS Nano.
Researchers
have known for several decades that electricity can be beneficial for skin
healing, but most electrotherapy units in use today require bulky electrical
equipment and complicated wiring to deliver powerful jolts of electricity.
“Acute
and chronic wounds represent a substantial burden in healthcare worldwide,”
says collaborator Angela Gibson, professor of surgery at UW–Madison and a burn
surgeon and director of wound healing services at UW Health.
“The use of electrical stimulation in wound healing is uncommon.”
“The use of electrical stimulation in wound healing is uncommon.”
In
contrast with existing methods, the new dressing is much more straightforward.
“Our
device is as convenient as a bandage you put on your skin,” says Wang.
The
new dressings consist of small electrodes for the injury site that are linked
to a band holding energy-harvesting units called nanogenerators, which are
looped around a wearer’s torso.
The natural expansion and contraction of the wearer’s ribcage during breathing powers the nanogenerators, which deliver low-intensity electric pulses.
The natural expansion and contraction of the wearer’s ribcage during breathing powers the nanogenerators, which deliver low-intensity electric pulses.
“The
nature of these electrical pulses is similar to the way the body generates an
internal electric field,” says Wang.
And,
those low-power pulses won’t harm healthy tissue like traditional, high-power
electrotherapy devices might.
In
fact, the researchers showed that exposing cells to high-energy electrical
pulses caused them to produce almost five times more reactive oxygen species —
major risk factors for cancer and cellular aging — than did cells that were
exposed to the nanogenerators.
Also
a boon to healing: They determined that the low-power pulses boosted viability
for a type of skin cell called fibroblasts, and exposure to the nanogenerator’s
pulses encouraged fibroblasts to line up (a crucial step in wound healing) and
produce more biochemical substances that promote tissue growth.
“These
findings are very exciting,” says collaborator Weibo Cai, a professor of
radiology at UW–Madison. “The detailed mechanisms will still need to be
elucidated in future work.”
In
that vein, the researchers aim to tease out precisely how the gentle pulses aid
in healing. The scientists also plan to test the devices on pig skin, which
closely mimics human tissue.
And,
they are working to give the nanogenerators additional capabilities—tweaking
their structure to allow for energy harvesting from small imperceptible
twitches in the skin or the thrumming pulse of a heartbeat.
“The
impressive results in this study represent an exciting new spin on electrical
stimulation for many different wound types, given the simplicity of the
design,” says Gibson, who will collaborate with the team to confirm the
reproducibility of these results in human skin models.
If
the team is successful, the devices could help solve a major challenge for
modern medicine.
“We
think our nanogenerator could be the most effective electrical stimulation
approach for many therapeutic purposes,” says Wang.
And
because the nanogenerators consist of relatively common materials, price won’t
be an issue.
“I
don’t think the cost will be much more than a regular bandage,” says Wang. “The
device in itself is very simple and convenient to fabricate.”
This
research was supported by grants from the National Institutes of Health
(R01EB021336 and P30CA014520).