GBD
study could benefit from more environmental health and climate change
estimates
 Recent
estimates in the Global Burden of Disease (GBD) study show that the combination
of air pollution, poor water sanitation and exposure to lead and radon is
responsible for 9 million premature deaths each year.
Recent
estimates in the Global Burden of Disease (GBD) study show that the combination
of air pollution, poor water sanitation and exposure to lead and radon is
responsible for 9 million premature deaths each year.
Yet
this figure captures only a fraction of the real burden of toxic pollutants in
the environment, and it doesn’t consider climate change, according to a
community of scientists led by researchers in the UW Department of
Environmental & Occupational Health Sciences (DEOHS) in the School of
Public Health.
In a new paper,
researchers highlight key challenges that limit the scope and accuracy of
current GBD estimates for environmental health risk factors and propose
strategies to clarify the true environmental footprint on health from chemical
pollution and climate change.
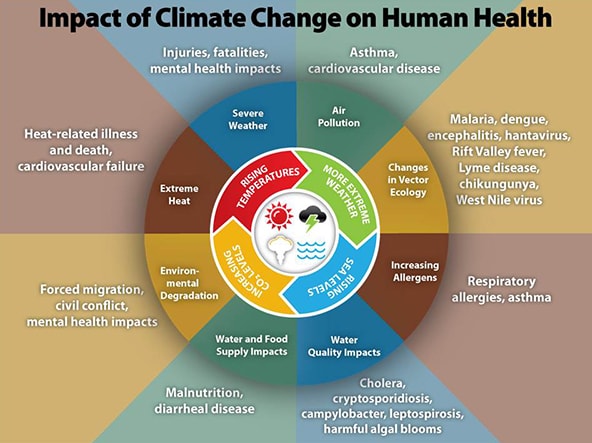
“There
are currently no GBD estimates related to a host of globally distributed toxic
pollutants or to climate change, which is arguably the greatest environmental
threat of them all,” said Dr. Howard Hu,
corresponding author and an affiliate professor in DEOHS.
Specifically,
climate change is not considered in a new type of GBD analysis, published in The Lancet in 2018, that forecasts
health and drivers of health on a global scale over the next 20 years.
One
reason for this is that climate change cannot easily be captured as a distinct
exposure, and there are unique data and modeling limitations, according to the
commentary. Additionally, “it is unclear what the baseline level for climate
risk should be, given its unique status as a constantly changing global
system,” the researchers wrote.
The
GBD—coordinated by the Institute for Health Metrics and Evaluation
(IHME)—provides a tool to quantify health loss from hundreds of diseases,
injuries and risk factors to help provide an evidence base for decision-making.
The GBD incorporated a limited set of climate risks in its 2000 analysis but
has since opted not to include climate risk in recent reports.
The
new GBD-Pollution and Health Initiative
To
close the gap in estimates of environmental health-related disease burden,
including those attributed to climate change, Hu and others came together to
form the GBD-Pollution and Health Initiative (PHI). The initiative involves key
partners from UW, IHME, the University of Toronto and the National Institute
for Environmental Health Sciences.
It
is based in DEOHS and draws on expertise from around the world, including
George Washington University’s Milken Institute School of Public Health,
Harvard T.H. Chan School of Public Health, McGill University and New York
University.
“The
thinking behind the initiative is that many countries, especially those that
are low- or middle-income and are striving to meet the United Nations’
Sustainable Development Goals, have the opportunity to avoid some of the
environmental tragedies that have plagued high-income countries and to engage
in ‘smart’ development,” Hu said.
“To
do so, policymakers need to know the identity, magnitude and potential
consequences of the environmental risk factors specific to their country.”
A
research agenda proposed in the commentary stems from a 2018 GBD-PHI workshop.
According to Hu, a workshop orchestrator, current GBD estimates only count
environmental impacts from air pollution, lead, radon and select occupational
exposures.
What
is missing are estimates related to climate change and other pollutants “that
are highly toxic, globally distributed and arguably having significant impacts
on health or functioning,” such as mercury, arsenic, pesticides, phthalates and
polychlorinated biphenyls or PCBs.
Measurement
challenges
Another
challenge is that most GBD data come from high-income countries, which have
lower levels of pollution compared to low- and middle-income countries.
Also,
current GBD metrics rely on outcomes that meet diagnostic criteria, “an
approach that lacks the ability to fully capture critical sub-clinical effects
such as moderate reductions in IQ from neurotoxicants like lead or mercury,” Hu
said.
Such
impacts are only counted in the GBD if IQ loss results in intellectual
disability (IQ less than 85). However, modest reductions in IQ are well known
to have major impacts on a person’s capacity for learning and the amount of
money they may make in their lifetime, upstream factors that could influence
health.
Since
sub-clinical effects have major implications for individuals and society but
are not fully captured by GBD methods, the commentary suggests, as an
alternative, measuring these effects based on other metrics such as those for
human capital developed recently by IHME and the World Bank. This metric was
described in The Lancet in 2018.
Collaboration
could lead to new data and methods
The
GBD-PHI is looking to leverage existing research and stimulate collaborations
with environmental health scientists, particularly those who can address the
lack of data on exposures to pollutants in low- and middle-income countries.
“We
share the desire to more completely capture the burden associated with
environmental risk factors, and we have continued to add new environmental risk
factors and new risk-outcome pairs with each new iteration of the GBD study,”
said Jeffrey Stanaway,
assistant professor of health metrics sciences at IHME and a co-author of the
commentary.
Said
Rachel Shaffer, lead author of the commentary and a DEOHS doctoral student in
environmental toxicology: "The GBD is highly influential in the global
public health policy arena. It is crucial that environmental exposures are more
fully incorporated and considered in future iterations of the GBD so
governments and policymakers can make appropriate decisions to allocate
resources and improve the health of their populations."