What the data shows on delaying the booster dose
William Petri, University of Virginia
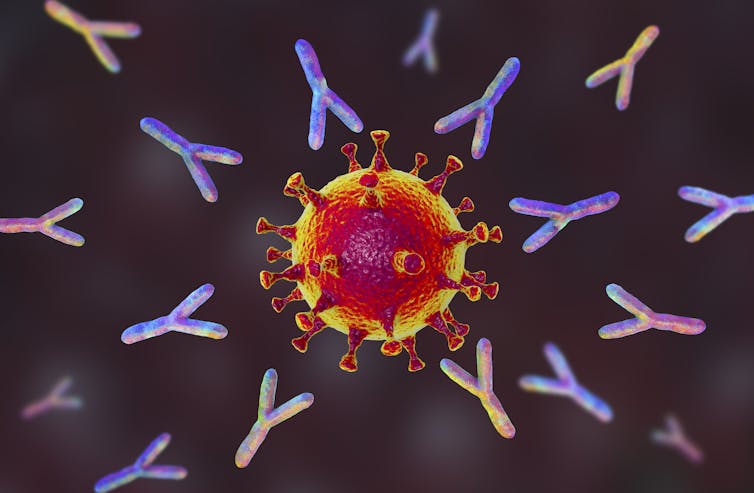 |
| After a second dose of the COVID-19 mRNA vaccine, a swarm of antibodies attacks the virus. Kateryna Kon/Science Photo Library via Getty Images |
As an infectious disease doctor, I’ve been fielding a lot of questions from my patients as well as my friends and family about whether the COVID-19 vaccine will still work if people are late receiving their second dose.
Why you need two doses 3-4 weeks apart
Two doses, separated by three to four weeks, is the tried-and-true approach to generate an effective immune response through vaccination, not just for COVID but for hepatitis A and B and other diseases as well.
The first dose primes the immune system and introduces the body to the germ of interest. This allows the immune system to prepare its defense. The second dose, or booster, provides the opportunity for the immune system to ramp up the quality and quantity of the antibodies used to fight the virus.
In the case of the Pfizer and Moderna COVID-19 vaccines, the second dose increases the protection afforded by the vaccine from 60% to approximately 95%.
Why the CDC decided receiving the second dose within 42 days is OK
In the clinical trial, the second dose of the Pfizer vaccine was administered as early as day 19 and as late as day 42 to 93% of the subjects. Since protection was approximately 95% for everyone who was vaccinated within this time “window,” there is little reason not to allow some flexibility in the timing of the second dose 2.
As more vaccine becomes available, the timing of the second dose should be close to four weeks for the Pfizer and Moderna vaccines. But the good news is that even while supplies remain limited, the science suggests that there’s nothing bad about getting a second dose as late as 42 days after the first.
What the immune system does between the first and second dose
The biology through which the mRNA vaccines induce their protection from COVID-19 is fundamentally different from that with other vaccines.
Pfizer and Moderna vaccines use messenger RNA that encodes the spike glycoprotein. Upon injection of the vaccine, the mRNA enters into immune cells called dendritic cells. The dendritic cells use the instructions written in the mRNA to synthesize the hallmark spike glycoprotein, which characterizes the SARS-CoV-2 virus that causes COVID-19. These immune cells then show the spike glycoprotein to B-cells, which then make anti-spike antibodies.
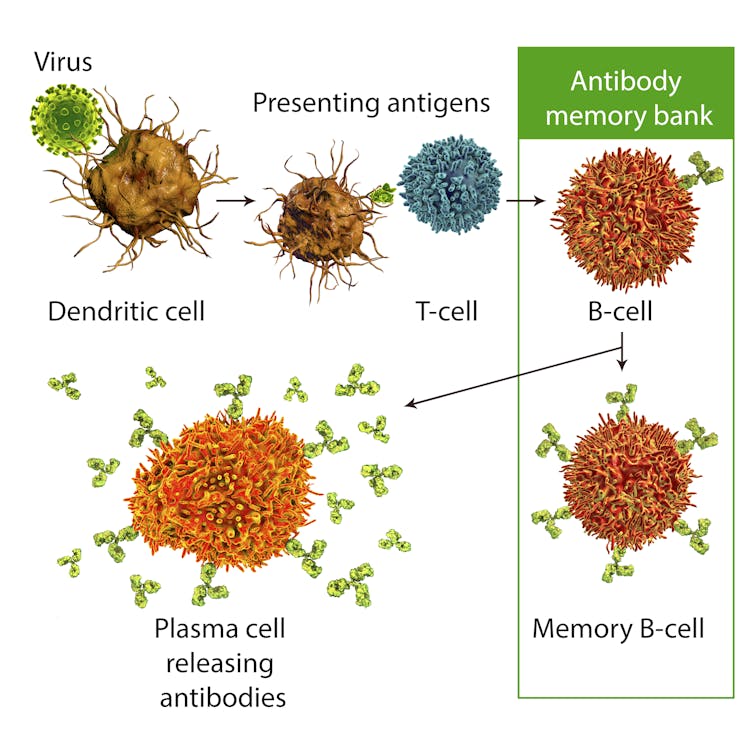
The mRNA vaccines are uniquely capable of inducing a special kind of immune cell – called a T-follicular helper cell – to help B-cells produce antibodies. The T-cells do this through direct contact with the B-cells and by sending chemical signals that tell the B-cells to produce antibodies. It is this help in antibody production that makes these vaccines so effective.
But not all B-cells are the same. There are two kinds that make anti-spike antibodies: long-lived plasma cells and memory B-cells. The long-lived plasma cells, as their name implies, live in the bone marrow for years after vaccination, continuously churning out antibody – in this case anti-spike antibody. These long-lived B-cells do not need to be boosted.
The memory B-cells, on the other hand, live in a state akin to hibernation. They do not produce antibodies until stimulated by a booster of the vaccine, or are exposed to infection with the coronavirus that causes COVID-19. That is the reason we need that second dose. Together these two types of B-cells provide a constant level of protection.
What happens if you don’t get the Pfizer or Moderna second dose on time?
With current vaccine shortages, and problems with setting up the infrastructure to vaccinate millions of people, many physicians are concerned that the second dose of vaccine won’t be delivered in the prescribed three-to-four-week window.
That booster shot is necessary for the T-cells to stimulate the memory B-cells to produce massive quantities of antibodies. If the booster isn’t given within the appropriate window, lower quantities of antibodies will be produced that may not provide as powerful protection from the virus.
[Deep knowledge, daily. Sign up for The Conversation’s newsletter.]![]()
William Petri, Professor of Medicine, University of Virginia
This article is republished from The Conversation under a Creative Commons license. Read the original article.