Emerging techniques could help detect the virus leading to cervical cancer
American Institute of Physics
Emerging technologies can screen for cervical cancer better than Pap smears and, if widely used, could save lives both in developing nations and parts of countries, like the United States, where access to health care may be limited.
In Biophysics Reviews, by AIP Publishing, scientists at Massachusetts General Hospital write advances in nanotechnology and computer learning are among the technologies helping develop HPV screening that take the guesswork out of the precancer tests.
That could mean better screening in places that lack highly
trained doctors and advanced laboratories.
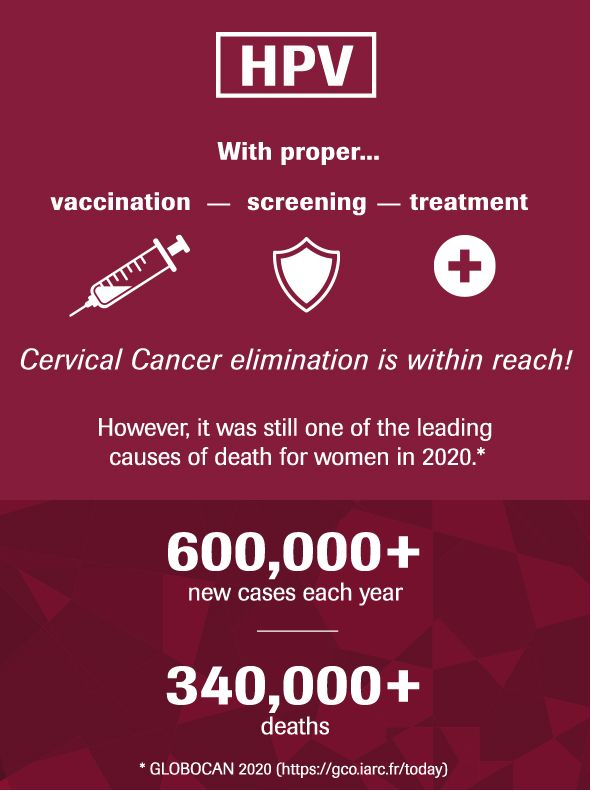
Cervical cancer is the world's fourth-most common cancer, with more than 500,000 cases diagnosed every year.
Almost all cases of cervical cancer are caused by HPV, or
human papillomavirus. Detecting precancer changes in the body gives doctors a
chance to cure what could otherwise become a deadly cancer.
Pap smears, which were introduced in the 1940s, are subjective and not always reliable.
The tests, which can detect about 80% of developing cervical cancer if given regularly, require high-quality laboratories, properly trained clinical doctors, and repeated screenings.
These test conditions are not widely available in many countries or even in low-income and remote parts of wealthier nations.
"The Pap smear has done wonders in terms of reducing mortality from a cancer that is very treatable when caught early and almost invariably fatal when it is caught late," said author Cesar Castro, an oncologist at Massachusetts General Hospital and associate professor at Harvard Medical School.
"And it is not
even a great test. Part of its imperfection is that there is subjectivity to
it. The trained eye is the limiting step in the process. The untrained eye, or
relatively untrained eye, can miss cancers."
The
subjectivity of the test has led to a much higher death rate from cervical
cancer in lower-income countries. The authors highlight a list of existing and
emerging technologies that can be used to close the testing gap in those areas.
They range from existing DNA testing and other Pap smear alternatives to
next-generation technologies that use recent advances in nanotechnology and
artificial intelligence.
One
technique involves screening with tiny beads made of biological material that
form a diamond shape when they contact HPV. Those shapes can be detected with
powerful microscopes. When those microscopes are not available, a mobile phone
app, built through machine learning, can be used to read them.
"Similar
to COVID-19 testing, we have great technology in places like the United States
that does not work well enough in other countries," said author Hyungsoon
Im, a biomedical engineer at Massachusetts General Hospital and assistant
professor at Harvard Medical School. "This is why there is great
motivation to find next-generation, affordable technology to address this
problem."