1. What We Now Know About the SARS-CoV-2 Delta Variant That’s Wreaking Havoc Globally
By
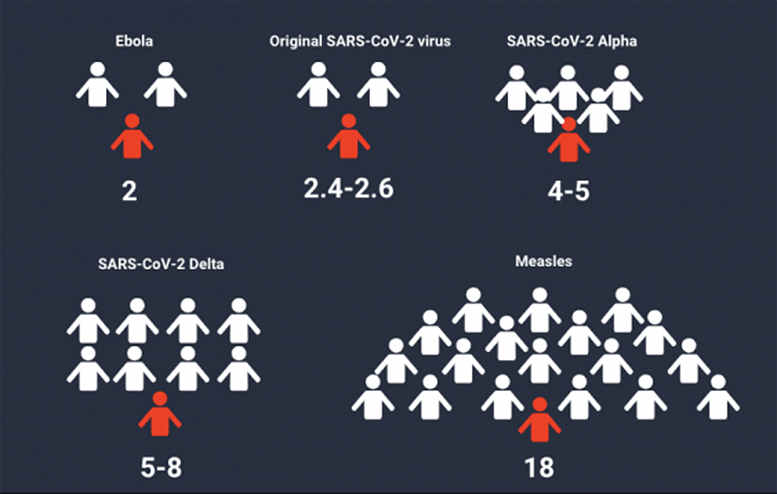 |
| The R0 (reproduction number) of SARS-CoV-2 variants and other diseases. The higher the R0 number, the more contagious the disease is. Credit: Imperial College London, Lancet, Australian Government. |
“It’s almost impossible to predict which variant will win the race and when we have reached the point of most transmissible,” said Dr. Di Giallonardo.
Natural selection has shaped the evolution of all living things on our planet, including viruses. While mutations emerge in viruses, some mutations have little impact while others outcompete other variants and persist, such as the SARS-CoV-2 variant, Delta – classified a variant of concern (VOC) by the World Health Organisation (WHO).Last week, Dr. Poonam Khetrapal Singh, the regional director of the WHO, South-East Asia said, “The Delta variant has spread to over a hundred countries and is likely to soon become the most dominant COVID-19 strain globally. Among the variants of concern, Delta spreads most rapidly.”
Researchers have indicated the Delta variant is the most transmissible variant yet — as much as 60 percent more contagious than the Alpha variant. However, there is limited research in terms of whether or not the Delta variant causes more severe illness than other variants.
The characterization of variants by the WHO came about in late 2020 as a result of variants that posed an increased risk to public health. These definitions assist in prioritizing global monitoring, research, and ultimately informing the ongoing response to the COVID-19 pandemic.
What is a variant of concern?
Currently, the Delta variant joins three other variants in this category – Alpha, which was first detected in the UK in September 2020; Beta, the earliest documented sample recorded in South Africa in May 2020; and Gamma, which had samples first documented in Brazil in November 2020.To be designated a VOC, a variant must meet the definition of a variant of interest (VOI).
This includes a variant:
- with genetic changes that are predicted or known to affect virus characteristics such as transmissibility, disease severity, immune escape, diagnostic or therapeutic escape; AND
- identified to cause significant community transmission or multiple COVID-19 clusters, in multiple countries with increasing relative prevalence alongside increasing number of cases over time, or other apparent epidemiological impacts to suggest an emerging risk to global public health.
To be ‘promoted’ to a VOC, the variant needs to have shown to be associated with one or more of the following changes at a degree of global public health significance:
- Increase in transmissibility or detrimental change in COVID-19 epidemiology; OR
- Increase in virulence or change in clinical disease presentation; OR
- Decrease in effectiveness of public health and social measures or available diagnostics, vaccines, therapeutics.
Will Delta outcompete the other variants of concern?
While the Delta variant continues to spread globally, where does this leave other variants of concern such as Alpha, Beta and Gamma? Will Delta eventually outcompete the others?Dr. Francesca Di Giallonardo, a virologist at The Kirby Institute at UNSW Sydney suggests this could potentially be the case.
“Most probably yes, as this is a common process in natural selection and immune escape. However, the timeline and characteristics of variant replacement may vary between different geographic regions, particularly in those isolated by border closures.
“Prediction of infectivity of new variants is not trivial. In general, viruses increase their transmissibility. That means that the most ‘successful in transmission’ variant outcompetes other variants. However, it’s almost impossible to predict which variant will win the race and when we have reached the point of most transmissible,” said Dr. Di Giallonardo.
According to Dr. Di Giallonardo, increased viral fitness is characterized by natural selection events. This means if variant B has replaced variant A, it must be fitter by definition, as B has outcompeted A. Most likely, variant B is antigenically distinct, which means it has escaped immune pressure.
“Such variants will keep emerging as immune selection is increased due to more people being vaccinated or infected,” said Dr. Di Giallonardo.
Are fitter variants likely to cause severe disease?
“New variants are fitter such that their replication and transmission capacity is better compared to the previous variants. There are numerous emerging variants that are region-specific and are seemingly not causing more severe disease.
“However, constant monitoring of such variants is crucial for identifying those that do indeed cause more severe disease. Thus, the WHO and CDC (Centres for Disease Control and Prevention) classify new emerging variants with a potential for increased severity as variants of concern and variants of interest.”
What is our best line of defense?
“Vaccinate, vaccinate, and vaccinate,” said Dr. Di Giallonardo. “We have a plethora of global data on the efficacy of the different vaccines. We know how effective they are in preventing severe disease and reducing transmission.”Virologist, Dr. Chantelle Ahlenstiel at the Kirby Institute said in terms of the mRNA vaccines such as Pfizer and Moderna, the sequences in the current vaccines – that tell the body how to make a specific type of virus spike protein – can be easily changed to match the newly emerging virus variant spike protein and could therefore provide protection against those too. Additionally, mRNA vaccines have the potential to be manufactured rapidly and inexpensively.
Surveillance is also critical for understanding which variants are circulating, as early identification will allow for rapid evaluation of vaccine efficacy.
“Surveillance means collecting data on the number of infections present for different virus variants, their geographic spread, and the associated disease severity. Such data is essential to better understand how variants spread across the states, country, and globally. We have more data for Covid-19 than for any other viral disease, thanks to systems which were already in place such as nexstrain.org, GISAID (Global Initiative on Sharing Avian Influenza Data),” said Dr. Di Giallonardo.
“Surveillance requires a tremendous amount of work and the global efforts have been great.”
By NORTHWESTERN UNIVERSITY
As breakthrough infections rise from the highly contagious Delta variant of the coronavirus, the precise risk to the fully vaccinated may be confusing.
Northwestern Medicine experts explain why the number of breakthrough infections from the Delta variant are going up, who is at risk and why you may need to take extra precautions depending on your age.
Who gets breakthrough infections?
Dr. Robert Murphy: “The vaccine is about 90% effective against the Delta variant, so one person in 10 who gets vaccinated and is exposed to SARS-CoV-2 will have a breakthrough infection. Anybody is at risk for it, not just the immune-compromised. It’s athletes. It’s totally healthy people. Certainly, the immune-compromised are at a higher risk because they can’t mount a strong enough immunologic response to the vaccine. Older people may also have a weaker response to the vaccine.
“The end game is most people who get breakthrough infections either have very mild symptoms or no symptoms. They rarely end up in the hospital, and they don’t die.
“The big question is how infectious are they? That’s what we are trying to find out.”
Murphy is the site leader at Northwestern along with Drs. Chad Achenbach and Claudia Hawkins in a study with the University of Illinois at Champaign and Johns Hopkins investigating the infectiousness of vaccinated students who got COVID-19 infections. Results are expected in the next one to two months.
Are we seeing more breakthrough infections from the Delta variant?
Carnethon: “We are seeing breakthrough infections and while we know that no vaccine is 100% effective, it feels frightening. However, infections will happen and the reassuring thing is that most of the breakthrough infections are not causing severe illness and death. We aren’t sure why the rate of infections — both new and breakthrough — appear to be picking up.
“One concern is the Delta variant is evading the vaccines. Another concern is any virus that causes a high viral load would break through vaccine protection — and there is evidence that the delta variant does cause higher viral loads earlier in the course of infection. We will never get away from these concerns because the virus will continue to mutate itself into new variants so long as it circulates in the population, and the biggest space it has to circulate is among the unvaccinated.”
Do we need to change our behavior now that the Delta variant is the main source of breakthrough infections?
Dr. Benjamin Singer: “In places with high vaccination rates and low community transmission, you do not need to change your behavior. Of course, vaccinated people may still choose to wear masks if they or someone in their household contact is at particularly high risk.
“But in places with low vaccination rates and high community transmission, I think it makes clear sense to add back masking when you are indoors as an additional layer of protection from a more contagious variant.
“Delta is a more contagious variant than previous SARS-CoV-2 variants and has a weak ability to evade vaccine immunity, at least among those who are only partially vaccinated with one dose of an mRNA vaccine. Hence, breakthrough infections may be more common with Delta.”
Mercedes Carnethon: “The Delta variant won’t change my behavior in a community where the test positivity rate remains low, which signals low community transmission. However, at this time I would not choose to travel to a hotspot. But if I had to go, I would wear my mask and try to avoid large groups of people. I would not take unvaccinated family members to a current hot spot or family members who are vaccinated but who remain vulnerable due to age or other conditions.”
“I have been following local guidance regarding mask-wearing and so feel comfortable indoors without a mask. The reason I have not returned to indoor mask-wearing in public spaces is because breakthrough infections have largely been minimally symptomatic or asymptomatic.
“If we have hit a wall on encouraging adults to vaccinate, then as a society, we have to shift our mindset to treating this as another endemic virus that is going to infect people every year just as the other coronaviruses that cause the common cold do each year. When a virus becomes endemic and infects and re-infects people over time, it does become less virulent with time. The number of unvaccinated individuals who are hospitalized right now with this new variant demonstrate that it is not yet mild and harmless.”
“Even still, operating under the same level of fear as we were last spring isn’t sustainable. It is also not necessary when we have considerable evidence that most vaccinated individuals who contract the illness do recover. There are still unknowns about long-term risks from infection or long-term COVID, but I can’t personally sustain that level of worry and anxiety over unknowns. I suspect many adults feel the same way. I have taken all the necessary precautions, but I won’t do dumb things like running around in a hot spot with no mask indoors.”
Should your behavior change if you are an older adult?
Carnethon: “All vulnerable individuals, either due to age or pre-existing conditions, should take precautions because if they are infected or re-infected it may not be a mild illness. The highest rates of mortality consistently have been older adults, which is traditionally defined as 65 and older. However, the risks for severe illness go up with each decade of life, and there is no age cutoff where the risk of illness is significantly lower. There are 40 year-olds with the health profiles that we know are associated with severe illness — obesity, diabetes, uncontrolled hypertension, cancer or pre-existing heart disease. Those individuals, regardless of their age, are just as vulnerable as older adults and should also take precautions.”
About the experts
Dr. Robert Murphy is executive director of the Institute for Global Health at Northwestern University Feinberg School of Medicine.
Mercedes Carnethon, vice chair of preventive medicine at Feinberg.
Dr. Benjamin Singer, assistant professor of medicine in pulmonary and critical care at Feinberg.
