Half of COVID survivors experience lingering symptoms six months after recovery
Penn State
More than half of the 236 million people who have been
diagnosed with COVID-19 worldwide since December 2019 will experience
post-COVID symptoms -- more commonly known as "long COVID" -- up to
six months after recovering, according to Penn State College of Medicine
researchers. 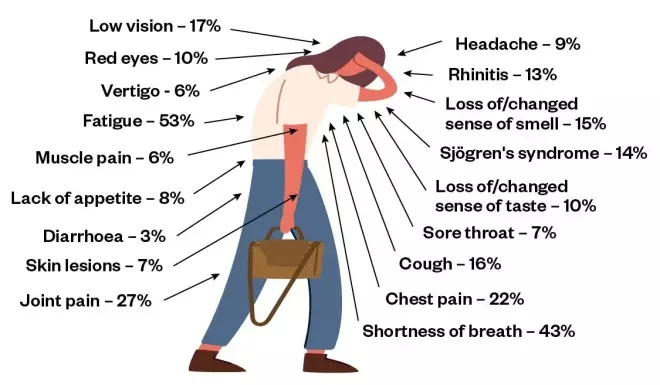
SOURCE: JAMA 2020;324(6):603-605
The research team said that governments, health care organizations
and public health professionals should prepare for the large number of COVID-19
survivors who will need care for a variety of psychological and physical
symptoms.
During their illnesses, many patients with COVID-19
experience symptoms, such as tiredness, difficulty breathing, chest pain, sore
joints and loss of taste or smell.
Until recently, few studies have evaluated patients' health after recovering from the coronavirus. To better understand the short- and long-term health effects of the virus, the researchers examined worldwide studies involving unvaccinated patients who recovered from COVID-19.
According
to the findings, adults, as well as children, can experience several adverse
health issues for six months or longer after recovering from COVID-19.
The researchers conducted a systematic review of 57 reports
that included data from 250,351 unvaccinated adults and children who were
diagnosed with COVID-19 from December 2019 through March 2021. Among those
studied, 79% were hospitalized, and most patients (79%) lived in high-income
countries. Patients' median age was 54, and the majority of individuals (56%)
were male.
The researchers analyzed patients' health post-COVID during three intervals at one month (short-term), two to five months (intermediate-term) and six or more months (long-term).
According to the findings, survivors experienced an array of residual health issues associated with COVID-19. Generally, these complications affected a patient's general well-being, their mobility or organ systems.
Overall, one in two survivors experienced long-term COVID manifestations. The
rates remained largely constant from one month through six or more months after
their initial illness.
The investigators noted several trends among survivors, such
as:
- General well-being: More than half of all patients reported weight loss, fatigue, fever or pain.
- Mobility: Roughly one in five survivors experienced a decrease in mobility.
- Neurologic concerns: Nearly one in four survivors experienced difficulty concentrating.
- Mental health disorders: Nearly one in three patients were diagnosed with generalized anxiety disorders.
- Lung abnormalities: Six in ten survivors had chest imaging abnormality and more than a quarter of patients had difficulty breathing.
- Cardiovascular issues: Chest pain and palpitations were among the commonly reported conditions.
- Skin conditions: Nearly one in five patients experienced hair loss or rashes.
- Digestive issues: Stomach pain, lack of appetite, diarrhea and vomiting were among the commonly reported conditions.
"These findings confirm what many health care workers and COVID-19 survivors have been claiming, namely, that adverse health effects from COVID-19 can linger," said co-lead investigator Vernon Chinchilli, chair of the Department of Public Health Sciences.
"Although previous
studies have examined the prevalence of long COVID symptoms among patients,
this study examined a larger population, including people in high-, middle- and
low-income countries, and examined many more symptoms. Therefore, we believe
our findings are quite robust given the available data."
"The burden of poor health in COVID-19 survivors is overwhelming," said co-lead investigator Dr. Paddy Ssentongo, assistant professor at the Penn State Center for Neural Engineering.
"Among these
are the mental health disorders. One's battle with COVID doesn't end with
recovery from the acute infection. Vaccination is our best ally to prevent
getting sick from COVID-19 and to reduce the chance of long-COVID even in the
presence of a breakthrough infection."
The mechanisms by which COVID-19 causes lingering symptoms in survivors are not fully understood. These symptoms could result from immune-system overdrive triggered by the virus, lingering infection, reinfection or an increased production of autoantibodies (antibodies directed at their own tissues).
The SARS-CoV-2 virus, the agent that causes COVID-19,
can access, enter and live in the nervous system. As a result, nervous system
symptoms such as taste or smell disorders, memory impairment and decreased
attention and concentration commonly occur in survivors.
"Our study was not designed to confirm COVID-19 as the
sole cause of these symptoms. It is plausible that symptoms reported by
patients in some of the studies examined were due to some other causes,"
said Ssentongo.
According to the researchers, early intervention will be
critical for improving the quality of life for many COVID-19 survivors. They
said that in the years ahead, health care providers will likely see an influx
of patients with psychiatric and cognitive problems, such as depression,
anxiety or post-traumatic stress disorder, who were otherwise healthy before
their COVID-19 infection. Based on these findings, health care providers should
plan and allocate resources accordingly in order to effectively monitor and
treat these conditions.
The research team noted that these long-term health
conditions may cause increased demand for medical care and could overwhelm
health care systems, particularly in low- and middle-income countries. They
said the findings from this study could help shape treatment plans to improve
care for COVID-19 patients and establish integrated evidence-based clinical
management for those affected.
"Since survivors may not have the energy or resources
to go back and forth to their health care providers, one-stop clinics will be
critical to effectively and efficiently manage patients with long COVID,"
Ssentongo said. "Such clinics could reduce medical costs and optimize
access to care, especially in populations with historically larger health care
disparities."
Destin Groff, Ashley Sun, Anna Ssentongo, Djibril Ba, Dr.
Alain Lekoubou; Dr. John Oh; and Dr. Jessica Ericson from Penn State College of
Medicine contributed to this research. Nicholas Parsons from Deakin University
and Govinda Poudel from Australian Catholic University in Australia also
contributed to this research.
The researchers declare no conflicts of interest or specific
funding for this research.