People of color, women and those with health conditions among veterans at high risk of food insecurity
Brown University
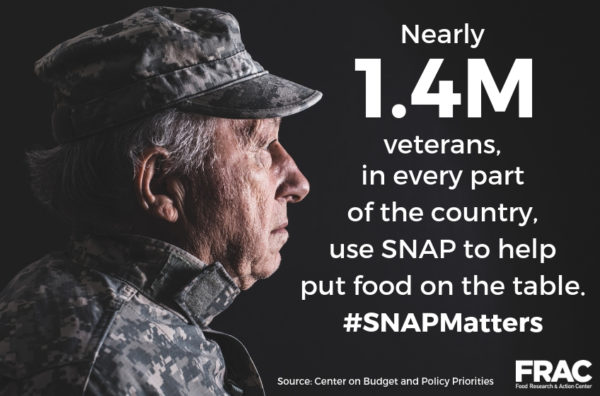
Up to 24% of U.S. military veterans are estimated to be affected by food insecurity — a limited or uncertain availability of nutritionally adequate food — and a new study found that risks are significantly higher for people of color and women.
It
also found that veterans with medical and trauma-related conditions as well as
unmet social needs like housing instability are more likely to experience food
insecurity.
For
the study, researchers at Brown University and the Providence V.A. Medical
Center analyzed data with a focus on revealing the characteristics of veterans
at the highest risk of food insecurity. If researchers know what populations to
target, tailored interventions can be developed to address their needs and
mitigate the long-term impacts of food insecurity on health and well-being.
“There’s not a one-size-fits-all solution for addressing veteran food insecurity,” said corresponding author Dr. Alicia Cohen, a Brown assistant professor (research) of family medicine and of health services, policy and practice. “So findings from studies like this can be used in many ways, from helping to identify the most at-risk groups to helping address veterans’ immediate food need to connecting veterans with programs and resources that can hopefully help improve their food security over the long term.”
Cohen
said that many veterans face economic and employment challenges following
military service, stemming both from service-related mental and physical health
issues as well difficulty reintegrating into civilian life —factors that can
increase the risk of food insecurity.
Yet
food insecurity is often missed in clinical settings, said Cohen, who is also a
primary care provider in the women’s health clinic and homeless clinic at the
Providence V.A. Medical Center. “You can’t tell by looking at a patient if
they're struggling to put food on the table,” she said.
And
like civilian patients, veterans often will not initiate a conversation with
their health care provider about their food needs.
“If
we don’t specifically ask veterans about their food needs, we are going to be
missing people who are experiencing hardship,” Cohen said. “There are a number
of resources within the V.A. and in the community to help address food
insecurity, but we can’t offer these resources if we don’t know that a veteran
is in need.”
That’s
one of the reasons the Veterans Health Administration developed a systematic
screening system in 2017 in which staff are prompted to ask veterans seeking
health care specifically about food insecurity. This new study is the first to
examine findings based on those screening questions. The researchers analyzed
data from the screenings to identify demographic and medical characteristics
associated with a positive food insecurity screen.
Between July 2017 and December 2018, 44,298 veterans screened positive for food insecurity. In their analysis, the researchers found that food insecurity was associated with identifying as non-Hispanic Black or Hispanic, non-married or partnered, and low-income. Veterans were also at higher risk for food insecurity if they had experienced homelessness or housing instability in the prior year, or if they had a diagnosis of diabetes, depression, and/or PTSD .
Prior military sexual trauma was associated with a significantly higher risk of food insecurity among both men and women. Notably, though, women screening positive for food insecurity were eight times more likely than men to have experienced military sexual trauma (49% of women vs. 6% of men).
This is a strong
example of how sexual trauma experienced while in the service can have a range
of serious downstream effects for veterans, Cohen said. “And as these results
show, women bear a much higher burden.”
As
a clinician who treats veterans, Cohen is familiar with how not having reliable
access to nutritious food can cause serious health problems and exacerbate
existing conditions. “I regularly see the negative impacts of food insecurity
on my patients,” she said.
Some
of the very factors that make veterans susceptible to food insecurity, like
diabetes or depression, can be worsened by not having healthy food to eat,
Cohen noted. The stress of not being able to afford food for oneself or one’s
family compounds the situation.
The study findings can inform the development of tailored, comprehensive interventions to address food insecurity among veterans, Cohen said. For example, if a clinician is treating a veteran with diabetes who is experiencing food insecurity, they can review the patient’s medical history to see if there are any medications they might have difficulty affording or that might put the veteran at risk for low blood sugar.
In a team-based model of care, the
clinician can refer the patient to a dietitian to provide nutritional
counseling based on the patient’s medical and social circumstances. V.A. social
workers can help meet a veteran’s immediate food need the day of their visit by
providing a meal ticket or referring them to a food pantry, as well as provide
assistance applying for any benefits for which they may qualify, such as
federal food assistance programs.
The
findings can also help start a conversation about refining screening practices,
Cohen said: “For example, they may help us identify specific groups that would
benefit from more targeted or more frequent screening for food insecurity, as
well as expanding where we conduct routine food insecurity screening to include
settings like mental health clinics.”
The
accepted manuscript was published online in Public Health Nutrition ahead of the
final version of the study that will appear in a print issue of the journal.
In
addition to Cohen, other Brown faculty who contributed to this research
included David Dosa, James Rudolph and Kali Thomas.
This
work was supported by grant CIN 13-419 from the V.A. Health Services Research
and Development Center of Innovation in Long Term Services and Supports, as
well as Department of Veterans Affairs Health Services Research and Development
grants CDA 20-037and CDA 14-422, and grant P30DK092926 from the National
Institute of Diabetes and Digestive and Kidney Diseases.