Researchers find a way to broaden the attack on COVID
By ROCKEFELLER UNIVERSITY PRESS
Researchers at Yale School of Medicine have discovered that
an RNA molecule that stimulates the body’s early
antiviral defense system can protect mice from a range of emerging SARS-CoV-2 variants. The study, published recently in
the Journal of Experimental Medicine (JEM), could lead to new treatments for COVID-19 in immunocompromised patients, as well as
providing an inexpensive therapeutic option for developing countries that
currently lack access to vaccines.
Though approved vaccines against SARS-CoV-2 are highly effective at preventing severe disease and death during the ongoing COVID-19 pandemic, vaccine availability is extremely limited in many low-income countries, and new, vaccine-resistant strains of the virus could emerge in the future.
Moreover, the vaccines’ effectiveness is already reduced in immunocompromised
individuals unable to form sufficient numbers of antibodies or T cells that
specifically target the viral spike protein. These individuals are susceptible
to chronic, long-term SARS-CoV-2 infections.
“This is why, in addition to the use of vaccines in preventing COVID-19, efforts are required to develop efficacious therapeutics against SARS-CoV-2,” says Akiko Iwasaki, a professor at Yale School of Medicine.
The body’s first line of defense against SARS-CoV-2—before the
involvement of antibodies and T cells—is thought to depend on receptor
molecules such as RIG-I that recognize the virus’s genetic material and induce
the production of signaling proteins known as type I interferons. These
interferons, in turn, promote the production of proteins that can inhibit viral
replication and stimulate the recruitment of immune cells to fight the
infection.
Multiple studies have suggested that early and robust production
of interferons protects against COVID-19, whereas delayed production is
associated with severe disease. A clinical trial has shown that treating
COVID-19 patients with purified interferon protein early during disease can
reduce mortality, but manufacturing interferons is extremely expensive.
In the new JEM study,
Iwasaki and colleagues suggest a cheaper alternative: treating patients with
short RNA molecules that mimic SARS-CoV-2’s genetic material and activate the
RIG-I receptor to stimulate production of type I interferons by the body’s own
cells.
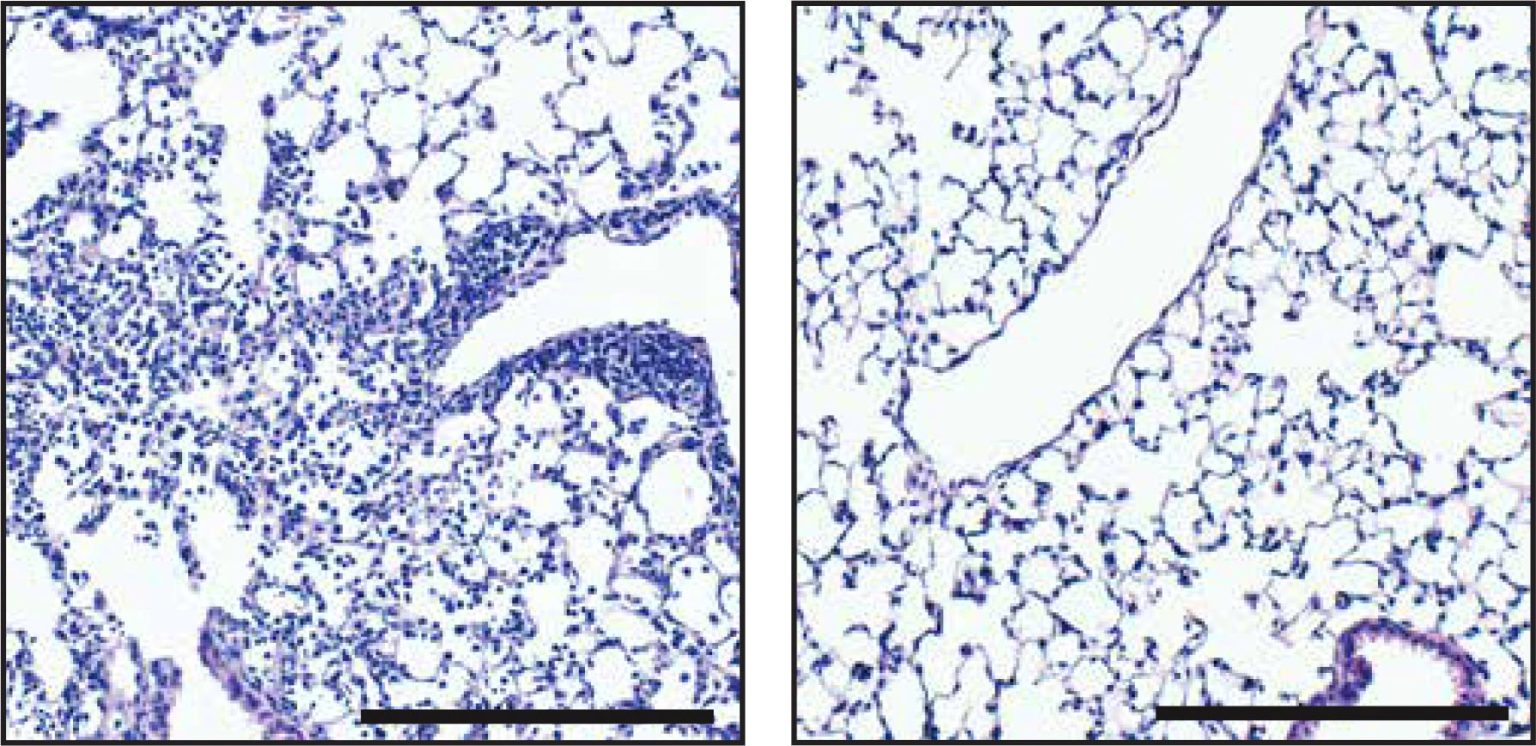
The researchers tested their approach in mice susceptible to
SARS-CoV-2 infection. A single dose of an RNA molecule named SLR14 was
sufficient to protect the mice from severe disease and death, particularly if
the treatment was provided shortly before or soon after exposure to the virus.
When administered shortly after viral infection, SLR14 was more effective than
treating mice with purified interferon protein, the researchers determined.
Crucially, SLR14 protected mice from all emerging SARS-CoV-2
variants, including the delta variant responsible for the recent surge in US
COVID-19 cases.
Finally, Iwasaki and colleagues tested SLR14 in
immunocompromised Rag–/– mice
chronically infected with SARS-CoV-2. The RNA molecule was able to completely
clear the virus from these animals, even though they lack both T cells and
antibody-producing B cells.
Iwasaki and colleagues point out that RNA molecules like SLR14 are
relatively cheap and easy to manufacture. “SLR14 therefore holds great promise
as a new class of RNA therapeutics that can be applied as antivirals against
SARS-CoV-2,” Iwasaki says. “Moreover, because this RNA-based therapeutic
approach is simple and versatile, our study will facilitate pandemic
preparedness and response against future respiratory pathogens sensitive to
type I interferons.”
Reference: ” A stem-loop RNA RIG-I agonist protects against acute
and chronic SARS-CoV-2 infection in mice” by Tianyang Mao, Benjamin Israelow,
Carolina Lucas, Chantal B.F. Vogels, Maria Luisa Gomez-Calvo, Olga Fedorova,
Mallery I. Breban, Bridget L. Menasche, Huiping Dong, Melissa Linehan, Yale
SARS-CoV-2 Genome Surveillance Initiative, Craig B. Wilen, Marie L. Landry,
Nathan D. Grubaugh, Anna M. Pyle and Akiko Iwasaki, 10 November 2021, Journal of Experimental Medicine (JEM).
DOI: 10.1084/jem.20211818