Over-stimulated immune system may be impetus to cognitive symptoms, study shows
University of California - San Francisco
Some patients who develop new cognitive symptoms after a mild bout of COVID have abnormalities in their cerebrospinal fluid similar to those found in people with other infectious diseases. The finding may provide insights into how SARS-CoV-2 impacts the brain.
In
a small study with 32 adults, comprising 22 with cognitive symptoms and 10
control participants without, researchers from UC San Francisco and Weill
Cornell Medicine, New York, analyzed the cerebrospinal fluid of 17 of the
participants who consented to lumbar puncture. All participants had had COVID
but had not required hospitalization.
They
found that 10 of 13 participants with cognitive symptoms had anomalies in their
cerebrospinal fluid. But all four of the cerebrospinal samples from
participants with no post-COVID cognitive symptoms were normal. The research
publishes on Jan. 18, 2022 in Annals of Clinical and Translational
Neurology.
The
average age of the participants with cognitive symptoms was 48, versus 39 for
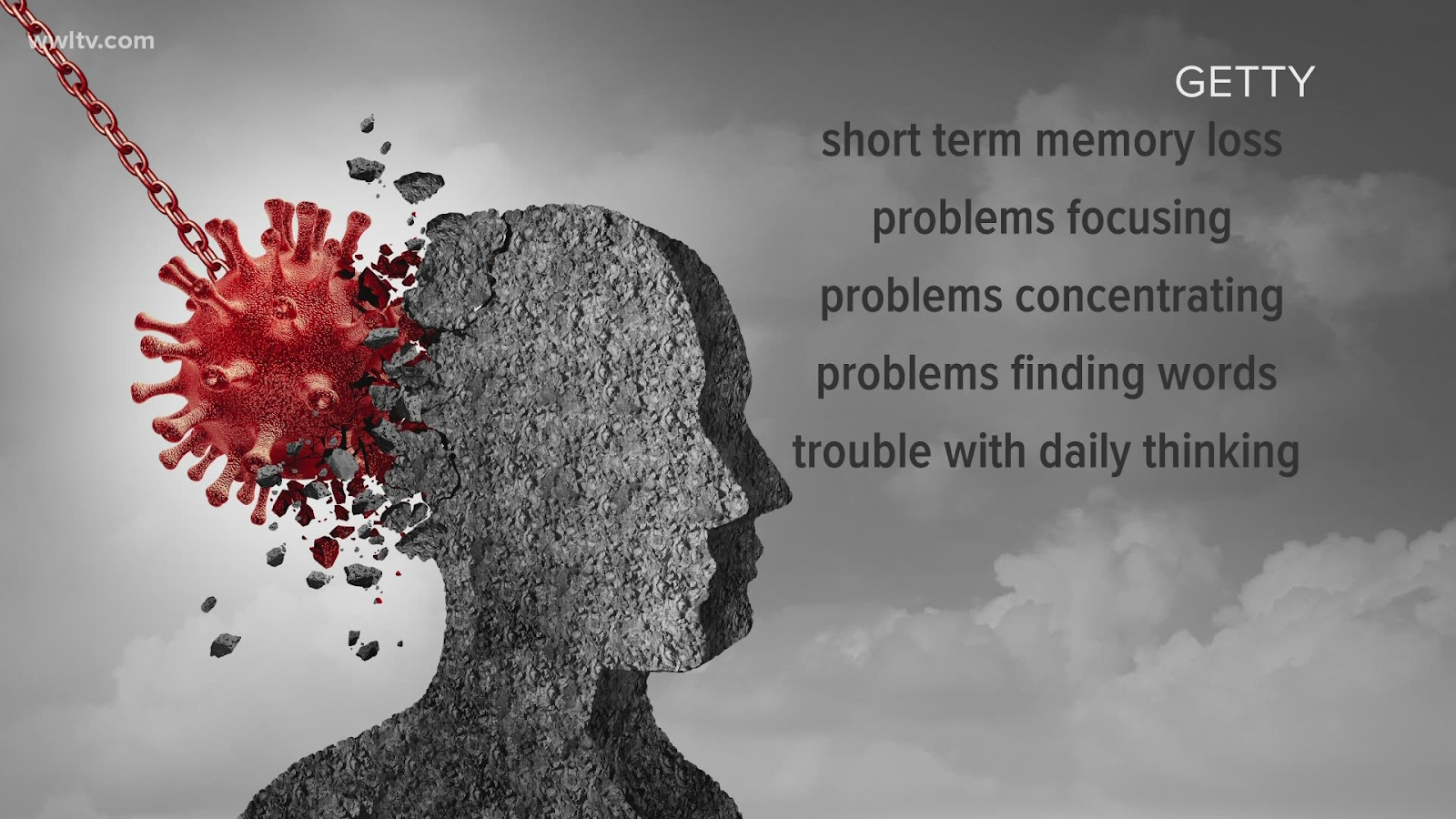
the control group. Participants with these symptoms presented with executive
functioning issues, said senior author Joanna Hellmuth, MD, MHS, of the UCSF
Memory and Aging Center. "They manifest as problems remembering recent
events, coming up with names or words, staying focused, and issues with holding
onto and manipulating information, as well as slowed processing speed,"
she said.
"Brain
fog" is a common after-effect of COVID, affecting some 67 percent of 156
patients at a post-COVID clinic in New York, a study published this month
shows. In the current study, patients were enrolled in the Long-term Impact of
Infection with Novel Coronavirus (LIINC) study that evaluates recovery in
adults with confirmed SARS-CoV-2.
Examinations of the cerebrospinal fluid revealed elevated levels of protein, suggesting inflammation, and the presence of unexpected antibodies found in an activated immune system. Some were found in the blood and cerebrospinal fluid, implying a systemic inflammatory response, or were unique to the cerebrospinal fluid, suggesting brain inflammation. While the targets of these antibodies are unknown, it is possible that these could be "turncoat" antibodies that attack the body itself.
Immune
System Runs Amok Months After COVID
"It's
possible that the immune system, stimulated by the virus, may be functioning in
an unintended pathological way," said Hellmuth, who is principal
investigator of the UCSF Coronavirus Neurocognitive Study and is also
affiliated with the UCSF Weill Institute for Neurosciences. "This would be
the case even though the individuals did not have the virus in their
bodies," she said, noting that the lumbar punctures took place on average
10 months after the participants' first COVID symptom.
The
researchers also found that the participants with cognitive symptoms had an
average of 2.5 cognitive risk-factors, compared with an average of less than
one risk factor for participants without the symptoms. These risk-factors
included diabetes and hypertension, which can increase the risk of stroke, mild
cognitive impairment and vascular dementia; and a history of ADHD, which may
make the brain more vulnerable to executive functioning issues. Other risk
factors included anxiety, depression, a history of heavy alcohol or repeated
stimulant use, and learning disabilities.
Testing
May Fall Short in Diagnosing Mild Cognitive Disorders
All
participants underwent an in-person cognitive testing battery with a
neuropsychologist, applying equivalent criteria used for HIV-associated
neurocognitive disorder (HAND). Surprisingly, the researchers found that 13 of
the 22 participants (59 percent) with cognitive symptoms met HAND criteria,
compared with seven of the 10 control participants (70 percent).
"Comparing cognitive performance to normative references may not identify
true changes, particularly in those with a high pre-COVID baseline, who may
have experienced a notable drop but still fall within normal limits," said
Hellmuth.
"If
people tell us they have new thinking and memory issues, I think we should
believe them rather than require that they meet certain severity
criteria."
Cognitive
symptoms have been identified in other viruses, in addition to COVID and HIV.
These include the coronaviruses SARS and MERS, hepatitis C and Epstein-Barr
virus.
Co-Authors: First
author is Alexandra C. Apple, PhD, of the UCSF Memory and Aging Center and the
Weill Institute for Neurosciences. For a complete list of co-authors, please
refer to the paper.
Funding
and Disclosures: The research is supported by grants from the
National Institutes of Health/NIMH (K23MH114724) and the National Institutes of
Health/NINDS (R01NS118995-14S). For a full list of disclosures, please refer to
the paper.