Haven’t had COVID yet? It could be more than just luck
Lindsay Broadbent, Queen's University Belfast
 |
| I Wei Huang/Shutterstock |
More than 60% of people in the UK have tested positive for COVID at least once. However, the number of people who have actually been infected with SARS-CoV-2, the virus that causes COVID-19, is thought to be higher. The calculated rate of asymptomatic infections varies depending on the study, though most agree it’s fairly common.
But even taking into account people who have had COVID and not realised it, there is still likely a group of people who never have. The reason why some people appear immune to COVID is one question that has persisted throughout the pandemic. As with so much in science, there isn’t (yet) one simple answer.
We can probably dismiss the Marvel-esque superpower theory. But science and luck likely both have a role to play. Let’s take a look.
The simplest explanation is that these people have never come into contact with the virus.
This could certainly be the case for people who have been shielding during the pandemic. People at significantly greater risk of severe disease, such as those with chronic heart or lung conditions, have had a tough couple of years.
Many of them continue to take precautions to avoid potential exposure to the virus. Even with additional safety measures, many of these people have ended up with COVID.
Due to the high level of community transmission, particularly with the extremely transmissible omicron variants, it’s very unlikely that someone going to work or school, socialising and shopping hasn’t been near someone infected with the virus. Yet there are people who have experienced high levels of exposure, such as hospital workers or family members of people who have had COVID, who have somehow managed to avoid testing positive.
We know from several studies vaccines not only reduce the risk of severe disease, but they can also cut the chance of household transmission of SARS-CoV-2 by about half. So certainly vaccination could have helped some close contacts avoid becoming infected. However, it’s important to note that these studies were done pre-omicron. The data we have on the effect of vaccination on omicron transmission is still limited.
Some theories
One theory around why certain people have avoided infection is that, although they are exposed to the virus, it fails to establish an infection even after gaining entry to the airways. This could be due to a lack of the receptors needed for SARS-CoV-2 to gain access to cells.
Once a person does become infected, researchers have identified that differences in the immune response to SARS-CoV-2 play a role in determining the severity of symptoms. It is possible that a quick and robust immune response could prevent the virus from replicating to any great degree in the first instance.
The efficacy of our immune response to infection is largely defined by our age and our genetics. That said, a healthy lifestyle certainly helps. For example, we know that vitamin D deficiency can increase the risk of certain infections. Not getting enough sleep can also have a detrimental effect on our body’s ability to fight invading pathogens.
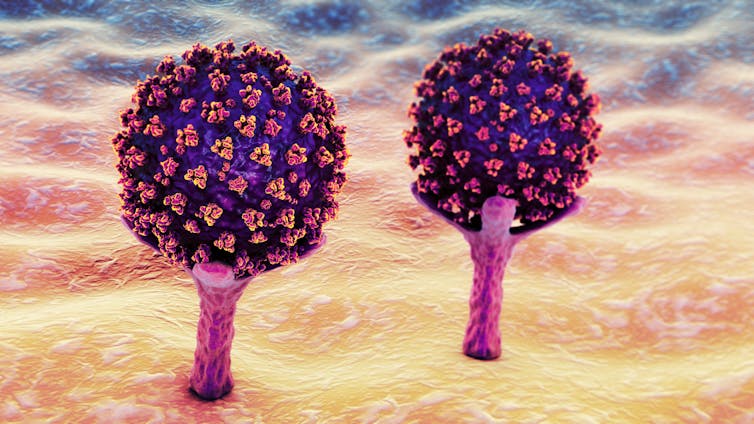 |
| The SARS-CoV-2 virus needs to attach to receptors to gain access to our cells. Kateryna Kon/Shutterstock |
Scientists studying the underlying causes of severe COVID have identified a genetic cause in nearly 20% of critical cases. Just as genetics could be one determining factor of disease severity, our genetic makeup may also hold the key to resistance to SARS-CoV-2 infection.
I research SARS-CoV-2 infection on nasal cells from human donors. We grow these cells on plastic dishes which we can then add virus to and investigate how the cells respond. During our research we found one donor whose cells could not be infected with SARS-CoV-2.
We discovered some really interesting genetic mutations, including several involved with the body’s immune response to infection, that could explain why. A mutation we identified in a gene involved with sensing the presence of a virus has previously been shown to confer resistance to HIV infection. Our research is on a small number of donors and highlights that we’re still only scraping the surface of research into genetic susceptibility or resistance to infections.
There’s also the possibility that previous infection with other types of coronaviruses results in cross-reactive immunity. This is where our immune system may recognise SARS-CoV-2 as being similar to a recent invading virus and launch an immune response. There are seven coronaviruses that infect humans: four that cause the common cold, and one each that cause Sars (severe acute respiratory syndrome), Mers (Middle East respiratory syndrome) and COVID.
How long-lasting this immunity may be is another question. Seasonal coronaviruses that circulated pre-2020 were able to reinfect the same people after 12 months.
If you’ve managed to avoid COVID to date, maybe you do have natural immunity to SARS-CoV-2 infection, or perhaps you’ve just been lucky. Either way, it’s sensible to continue to take precautions against this virus that we still know so little about.![]()
Lindsay Broadbent, Research Fellow, School of Medicine, Dentistry and Biomedical Sciences, Queen's University Belfast
This article is republished from The Conversation under a Creative Commons license. Read the original article.