Vaccines Only Offer Modest Protection Against Long COVID
By
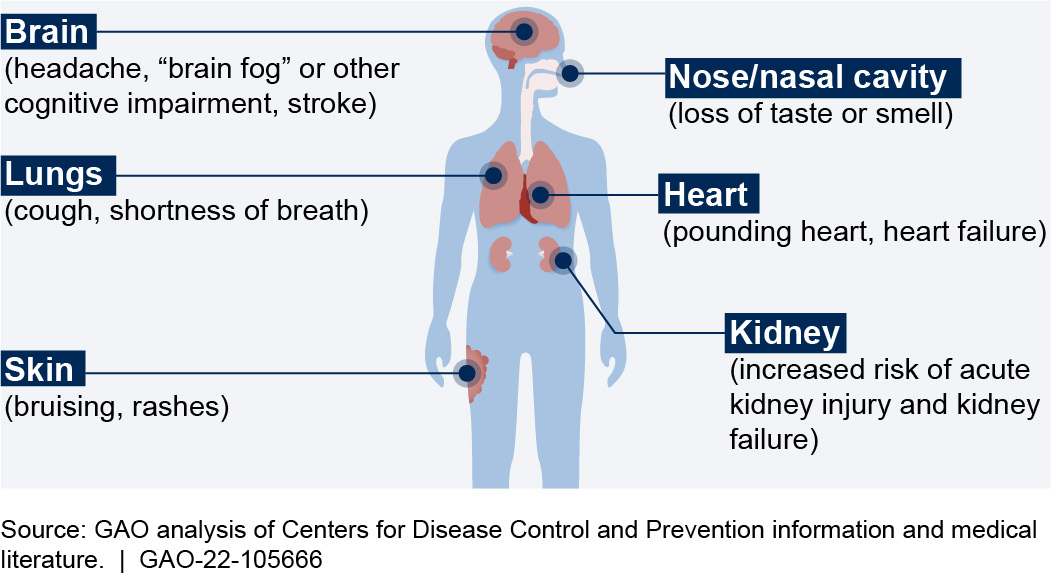
New research reveals that even vaccinated people with mild breakthrough COVID-19 infections can experience debilitating, lingering long COVID symptoms that affect the heart, brain, lungs, and other parts of the body.While risks are higher for the unvaccinated, a new study points to the need for more tools against the virus.
According to researchers at Washington University School of Medicine in St. Louis and the Veterans Affairs St. Louis Health Care System, vaccinated people with mild breakthrough COVID-19 infections can experience debilitating, lingering symptoms affecting the heart, brain, lungs, and other parts of the body.
A new study of more than 13 million veterans, however, discovered that immunization against the virus that causes COVID-19 lowered the chance of mortality by 34% and the likelihood of developing long COVID-19 by 15% when compared to unvaccinated individuals infected with the virus.
Even vaccinated people with mild breakthrough COVID-19 infections can experience persistent debilitating symptoms that affect the heart, brain, lungs, and other parts of the body, according to new research from Washington University School of Medicine in St. Louis and the Veterans Affairs St. Louis Health Care System.
“Vaccinations remain critically important in the fight against COVID-19.” — Ziyad Al-Aly, MD
The analysis of more than 13 million veterans also found that vaccination against the SARS-CoV-2 virus that causes COVID-19 reduced the risk of death by 34% and the risk of getting long COVID by 15%, compared with unvaccinated patients infected with the coronavirus. However, vaccines were shown to be most effective in preventing some of the most worrisome manifestations of long COVID – lung and blood-clotting disorders – which declined about 49% and 56%, respectively, among those who were vaccinated.
The research was published on May 25, 2022, in the journal Nature Medicine.
“Vaccinations remain critically important in the fight against COVID-19,” said first author Ziyad Al-Aly, MD, a clinical epidemiologist at Washington University. “Vaccinations reduce the risk of hospitalization and dying from COVID-19. But vaccines seem to only provide modest protection against long COVID. People recovering from breakthrough COVID-19 infection should continue to monitor their health and see a health-care provider if lingering symptoms make it difficult to carry out daily activities.”
The researchers classified patients as fully vaccinated if they had received two doses of the Moderna or Pfizer-BioNTech vaccines or one dose of the Johnson & Johnson/Janssen vaccine. At the time the research was conducted, the database used for this study did not include information about whether patients received boosters.
“Now that we understand that COVID-19 can have lingering health consequences even among the vaccinated, we need to move toward developing mitigation strategies that can be implemented for the longer term since it does not appear that COVID-19 is going away any time soon,” said Al-Aly, who is also the chief of research and development at the VA St. Louis Health Care System. “We need to urgently develop and deploy additional layers of protection that could be sustainably implemented to reduce the risk of long COVID.”
Such protective layers could include nasal vaccines that are more convenient or powerful than the current injections, or other types of vaccines or drugs aimed at minimizing the risks of long COVID.
“Getting COVID-19, even among vaccinated people, seems almost unavoidable nowadays,” said Al-Aly, noting that 8 to 12% of vaccinated people with breakthrough infections may develop long COVID. “Our current approach will likely leave a large number of people with chronic and potentially disabling conditions that have no treatments. This will not only affect people’s health, but their ability to work, life expectancy, economic productivity, and societal well-being. We need to have a candid national conversation about the consequences of our current approach.”
Since the pandemic started, more than 524 million people globally have been infected with the virus; of those, more than 6 million have died – including more than 1 million in the United States alone.
“Let’s say SARS-CoV-2 is here for 10 years,” Al-Aly continued. “People are sick and tired of masking and social distancing, and it’s simply not sustainable to ask that they continue to do so. We need to come up with additional layers of protection that allow us to resume normal life while co-existing with the virus. Current vaccines are only part of the solution.”
For the study, researchers analyzed the de-identified medical records of more than 13 million veterans. The records are in a database maintained by the U.S. Department of Veterans Affairs, the nation’s largest integrated healthcare delivery system. The researchers examined data of 113,474 unvaccinated COVID-19 patients and 33,940 vaccinated patients who had experienced COVID-19 breakthrough infections, all from Jan. 1 through Oct. 31, 2021.
The patients with COVID-19 were mostly older, white men; however, the researchers also analyzed data that included more than 1.3 million women and adults of all ages and races.
The study does not include data involving the virus’s omicron variants, which began spreading rapidly in late 2021. However, Al-Aly said prior studies have suggested the vaccine is effective against all current variants.
Among the study’s other findings:
In addition to complications involving the heart, brain, and lungs, other symptoms associated with long COVID included disorders involving the kidneys, blood clotting, mental health, metabolism, and the gastrointestinal and musculoskeletal systems.
Long COVID risks were 17% higher among vaccinated immunocompromised people with breakthrough infections compared with previously healthy, vaccinated people who experienced breakthrough infections.
An analysis of 3,667 vaccinated patients who were hospitalized with breakthrough COVID-19 infections showed that they experienced 2.5 times the risk of death than people who were hospitalized with influenza. They also had a 27% higher risk of long COVID in the first 30 days after diagnosis compared with 14,337 people who were hospitalized with seasonal influenza.
The datasets also compared long-term health outcomes with a pre-pandemic control group of more than 5.75 million people (meaning they had never had COVID-19 because it hadn’t yet existed). Across the board, people who had breakthrough COVID-19 faced significantly higher risks of death and illnesses such as heart and lung diseases, neurological conditions, and kidney failure.
“The constellation of findings shows that the burden of death and disease experienced by people with breakthrough COVID-19 infections is not trivial,” Al-Aly said.
Reference: “Long COVID after breakthrough SARS-CoV-2 infection” by Ziyad Al-Aly, Benjamin Bowe and Yan Xie, 25 May 2022, Nature Medicine.
DOI: 10.1038/s41591-022-01840-0
This research was funded by the U.S. Department of Veterans Affairs; the American Society of Nephrology; and KidneyCure.
Even vaccinated people with mild breakthrough COVID-19 infections can experience persistent debilitating symptoms that affect the heart, brain, lungs, and other parts of the body, according to new research from Washington University School of Medicine in St. Louis and the Veterans Affairs St. Louis Health Care System.
“Vaccinations remain critically important in the fight against COVID-19.” — Ziyad Al-Aly, MD
The analysis of more than 13 million veterans also found that vaccination against the SARS-CoV-2 virus that causes COVID-19 reduced the risk of death by 34% and the risk of getting long COVID by 15%, compared with unvaccinated patients infected with the coronavirus. However, vaccines were shown to be most effective in preventing some of the most worrisome manifestations of long COVID – lung and blood-clotting disorders – which declined about 49% and 56%, respectively, among those who were vaccinated.
The research was published on May 25, 2022, in the journal Nature Medicine.
“Vaccinations remain critically important in the fight against COVID-19,” said first author Ziyad Al-Aly, MD, a clinical epidemiologist at Washington University. “Vaccinations reduce the risk of hospitalization and dying from COVID-19. But vaccines seem to only provide modest protection against long COVID. People recovering from breakthrough COVID-19 infection should continue to monitor their health and see a health-care provider if lingering symptoms make it difficult to carry out daily activities.”
The researchers classified patients as fully vaccinated if they had received two doses of the Moderna or Pfizer-BioNTech vaccines or one dose of the Johnson & Johnson/Janssen vaccine. At the time the research was conducted, the database used for this study did not include information about whether patients received boosters.
“Now that we understand that COVID-19 can have lingering health consequences even among the vaccinated, we need to move toward developing mitigation strategies that can be implemented for the longer term since it does not appear that COVID-19 is going away any time soon,” said Al-Aly, who is also the chief of research and development at the VA St. Louis Health Care System. “We need to urgently develop and deploy additional layers of protection that could be sustainably implemented to reduce the risk of long COVID.”
Such protective layers could include nasal vaccines that are more convenient or powerful than the current injections, or other types of vaccines or drugs aimed at minimizing the risks of long COVID.
“Getting COVID-19, even among vaccinated people, seems almost unavoidable nowadays,” said Al-Aly, noting that 8 to 12% of vaccinated people with breakthrough infections may develop long COVID. “Our current approach will likely leave a large number of people with chronic and potentially disabling conditions that have no treatments. This will not only affect people’s health, but their ability to work, life expectancy, economic productivity, and societal well-being. We need to have a candid national conversation about the consequences of our current approach.”
Since the pandemic started, more than 524 million people globally have been infected with the virus; of those, more than 6 million have died – including more than 1 million in the United States alone.
“Let’s say SARS-CoV-2 is here for 10 years,” Al-Aly continued. “People are sick and tired of masking and social distancing, and it’s simply not sustainable to ask that they continue to do so. We need to come up with additional layers of protection that allow us to resume normal life while co-existing with the virus. Current vaccines are only part of the solution.”
For the study, researchers analyzed the de-identified medical records of more than 13 million veterans. The records are in a database maintained by the U.S. Department of Veterans Affairs, the nation’s largest integrated healthcare delivery system. The researchers examined data of 113,474 unvaccinated COVID-19 patients and 33,940 vaccinated patients who had experienced COVID-19 breakthrough infections, all from Jan. 1 through Oct. 31, 2021.
The patients with COVID-19 were mostly older, white men; however, the researchers also analyzed data that included more than 1.3 million women and adults of all ages and races.
The study does not include data involving the virus’s omicron variants, which began spreading rapidly in late 2021. However, Al-Aly said prior studies have suggested the vaccine is effective against all current variants.
Among the study’s other findings:
In addition to complications involving the heart, brain, and lungs, other symptoms associated with long COVID included disorders involving the kidneys, blood clotting, mental health, metabolism, and the gastrointestinal and musculoskeletal systems.
Long COVID risks were 17% higher among vaccinated immunocompromised people with breakthrough infections compared with previously healthy, vaccinated people who experienced breakthrough infections.
An analysis of 3,667 vaccinated patients who were hospitalized with breakthrough COVID-19 infections showed that they experienced 2.5 times the risk of death than people who were hospitalized with influenza. They also had a 27% higher risk of long COVID in the first 30 days after diagnosis compared with 14,337 people who were hospitalized with seasonal influenza.
The datasets also compared long-term health outcomes with a pre-pandemic control group of more than 5.75 million people (meaning they had never had COVID-19 because it hadn’t yet existed). Across the board, people who had breakthrough COVID-19 faced significantly higher risks of death and illnesses such as heart and lung diseases, neurological conditions, and kidney failure.
“The constellation of findings shows that the burden of death and disease experienced by people with breakthrough COVID-19 infections is not trivial,” Al-Aly said.
Reference: “Long COVID after breakthrough SARS-CoV-2 infection” by Ziyad Al-Aly, Benjamin Bowe and Yan Xie, 25 May 2022, Nature Medicine.
DOI: 10.1038/s41591-022-01840-0
This research was funded by the U.S. Department of Veterans Affairs; the American Society of Nephrology; and KidneyCure.