Research shows that a cancer-seeking molecule can successfully target bladder cancer with diagnostic and therapeutic agents
By
Kevin
Stacey
A research team from the University of Rhode Island and The Miriam
Hospital in Providence has demonstrated a potential new weapon in the fight
against bladder cancer.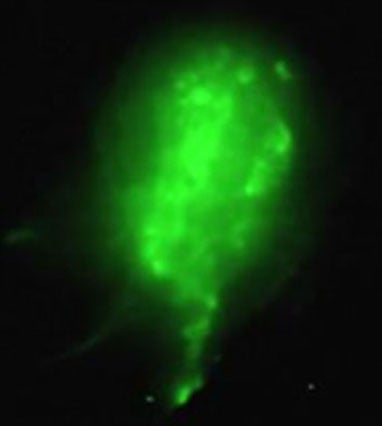
pHLIP-ICG can locate cancerous lesions and illuminate them
with a fluorescent molecule, making them potentially easier
for surgeons to see and remove.
The researchers showed that a cancer-seeking molecule called pHLIP used in combination with an FDA-approved fluorescent dye called ICG can successfully target tumors in human bladders, lighting up cancerous lesions to make them easier for surgeons to see and remove. In a separate experiment reported in the same study, the researchers showed that pHLIP® peptides combined with a powerful toxin called amanitin could penetrate and kill bladder cancer cells in a petri dish.
The researchers say the findings could set the stage for a
potential clinical trial to test the effectiveness of pHLIP-based treatments in
patients with non-muscle invasive bladder cancer.
“Bladder cancer can be a devastating disease, and case rates are
rising particularly here in Rhode Island,” said Yana Reshetnyak, a physics
professor at URI and a study co-author. “Our results suggest that pHLIP
peptides could potentially be used to aid in fluorescence-guided surgeries or
in targeting therapeutics to bladder and perhaps other urinary tract cancers.”
The study is published in the journal Frontiers in Urology.
A cancer-seeking peptide
Reshetnyak and Oleg Andreev, also a physics professor at URI, have been
developing pHLIP technology as a potential cancer-fighter since 2004, as part
of an ongoing collaboration with biophysicist Donald Engelman of Yale. The
molecule targets cancer cells through their acidity, which is a hallmark of
malignant tumors. While the area surrounding healthy cells has a fairly neutral
pH of around 7.4, cancer cells have a much lower pH between 5.5 and 6.5 (lower
numbers indicate more acidity) in their vicinity.
The pHLIP (short of pH-Low Insertion Peptide) molecule is derived
from bacteriorhodopsin, a membrane protein that enables some single-celled
organisms to convert light to energy. Bacteriorhodopsin consists of seven
peptide helices bound together in a protein complex. Experiments by Engelman
showed that one of those helices—which would eventually become known as
pHLIP—could only cross a cell membrane when the surrounding pH is low. When
Reshetnyak joined Engelman’s lab as a postdoctoral researcher in 2003, she got
the idea to try using this helix to seek out cancer cells.
“We knew that cancer cells tend to be acidic, and here we had this
peptide that only crosses a cell membrane when the pH is low,” Reshetnyak said.
“That’s when we started thinking this might be useful in cancer treatment.”
She worked with Andreev and Engelman to further study the peptide,
showing that it can indeed target cancer cells while leaving surrounding
healthy cells untouched. They also showed that they could attach other
molecules to pHLIP—chemotherapy drugs, immuno-modulating drugs, or fluorescent
molecules useful for tumor imaging. The pHLIP peptide could then deliver those
molecules directly to cancer cells and either tether them to cell surface or
escort them through the cell membrane.
A new weapon against bladder cancer
To test whether pHLIP agents might be helpful in treating bladder cancer, the
pHLIP team worked with Dr. Dragan Golijanin, director of Genitourinary Oncology
at The Miriam Hospital.
Golijanin’s team selected 26 patients whose bladders needed to be
removed as part of their cancer treatment. After the bladders were removed, his
team injected a solution of pHLIP® molecules
combined with a fluorescent molecule ICG. Golijanin then used a cystoscope, a
small camera placed in the bladder, to examine the inside of each bladder. The
experiment showed that pHLIP-ICG illuminated tumors with high specificity and
sensitivity. In fact, pHLIP-ICG improved cancer detection by 17% compared to a
widely used diagnostic method.
Golijanin says the results suggest that pHLIP-ICG has potential
for fluorescence-guided surgery. Not only does it find tumors that other
techniques miss, it also works faster than other methods, making pHLIP-ICG
potentially more practical for use in the operating room.
“We showed that you could potentially do cystoscopy by injecting
pHLIP-ICG about 15 minutes before the procedure, and you can see all the
malignant lesions,” Golijanin said. “This could give us better cancer clearance
and better resection of tumors at the time of cystoscopy. And it’s much less
cumbersome than other methods that take at least an hour, which is not a
pleasant waiting time for the patient.”
The results expand pHLIP-ICG’s promise in fluorescence-guided
surgery. A phase 1 fluorescence-guided surgical clinical trial on breast cancer
patients is currently underway at the Memorial Sloan Kettering Cancer Center in
New York City. These new results suggest that pHLIP-ICG could also aid in
bladder cancer surgeries.
For the second part of the research, the team tested pHLIP combined
with amanitin, a toxin derived from mushrooms. Using several different types of
breast and bladder cancer cell lines, the experiments showed that
pHLIP-amanitin was able to penetrate and kill cancer cells when their pH was
low. Those results suggest that pHLIP-amanitin can successfully target and kill
malignant lesions while minimizing effects on surrounding cells with normal pH.
A phase one clinical trial led by Cybrexa Therapeutics, is
currently testing pHLIP linked to another cytotoxic drug, exatecan. These new
results suggest that pHLIP-amanitin could be another potential therapeutic
combination.
Taken together, the researchers say, the results suggest that
pHLIP could be useful in diagnosis as well as surgical and therapeutic
treatments of bladder cancer.
“This approach to imaging and the approach to treatment go
hand-in-hand because they follow the sample principle,” Golijanin said. “I
think it has the potential to revolutionize how we treat non-muscle-invasive
bladder cancer.”
The research was supported by the National Institutes of Health
(R01GM073857, R01CA203737) and a Feibelman Family research grant. The phase one
fluorescence-guided surgery clinical trial (NCT05130801) measures safety of
escalating doses of pHLIP-ICG is tested, as well as agent performance in
operating room for identification of cancerous lesions using fluorescent
imaging instrument provided by Stryker Corp.