Pill-sized monitor gives unique information about digestive health
University of California - San Diego
Engineering researchers have developed a battery-free,
pill-shaped ingestible biosensing system designed to provide continuous
monitoring in the intestinal environment. It gives scientists the ability to
monitor gut metabolites in real time, which wasn't possible before. This feat
of technological integration could unlock new understanding of intestinal
metabolite composition, which significantly impacts human health overall.
The work, led by engineers at the University of California San
Diego, appears in the December issue of the journal Nature
Communications.
The ingestible, biofuel-driven sensor facilitates in-situ access
to the small intestine, making glucose monitoring easier while generating
continuous results. These measurements provide a critical component of tracking
overall gastrointestinal health, a major factor in studying nutrition,
diagnosing and treating various diseases, preventing obesity, and more.
"In our experiments, the battery-free biosensor technology continuously monitored glucose levels in the small intestines of pigs 14 hours after ingestion, yielding measurements every five seconds for two to five hours," said Ernesto De La Paz Andres, a nanoengineering graduate student at UC San Diego and one of the co-first authors on the paper. "Our next step is to reduce the size of the pills from the current 2.6 cm in length so they will be easier for human subjects to swallow."
Older methods for directly monitoring the inside of the small
intestine can cause significant discomfort for patients while generating only
single short data recordings of an environment that continuously changes. By
contrast, this biosensor provides access to continuous data readings over time.
The platform could also be used to develop new ways to study the microbiome of
the small intestine. The "smart pill" approach could lead to simpler
and cheaper ways to monitor the small intestine, which could lead to
significant cost savings in the future.
"Currently, the way to sample fluid inside the stomach and
intestines is to do an endoscopy, where a catheter is inserted down your throat
and into your GI tract by a doctor," said Patrick Mercier, a professor of
electrical and computer engineering at UC San Diego who led the team along with
nanoengineering professor Joseph Wang. Wang and Mercier co-direct the UC San
Diego Center for Wearable Sensors. "By combining the ultra-low-power
circuit and wireless technologies from my lab with glucose-powered fuel cell
and cutting-edge electrochemical sensing from the lab of UC San Diego
nanoengineering professor Joseph Wang, we have an opportunity to create new
modalities for understanding what is happening in the small intestine,"
said Mercier.
Instead of a battery, this "smart pill" is powered by
a non-toxic fuel cell that runs on glucose.
"With our battery-free smart pill approach, we have
opportunities to monitor the small intestine for much longer than just a
moment," said Wang. "We also plan to add additional sensors to the
system. Our goal is to develop a sensing platform for the intestine that allows
for the collection of many different kinds of information over longer periods
of time. We are working to show that there is so much opportunity to discover what
is really happening in the small intestine. I hope this kind of information
will be useful for better understanding the role that changes in the small
intestine environment play in health and disease."
A smarter way to measure critical intestinal activity
Approximately 20% of us will suffer from gastrointestinal
disorders at some point in our lives. These may include inflammatory bowel
disease (IBD), diabetes or obesity, all caused, in part, by the dysfunction of
the intestinal processes involving the absorption or digestion of gut
metabolites. Such maladies represent a significant cost to the economy and
strain on healthcare systems. Therefore, the stakes of accessing information
from the relevant sections of the GI tract are quite high.
However, there are significant challenges to developing
ingestible sensors such as the new smart pill system developed at UC San Diego.
"It has proven difficult to create an ingestible device
equipped with the necessary sensors and electronics to perform wireless readout
and doesn't need batteries," said Wang.
To address these specifications, the team landed on a
self-powered glucose biofuel biosensor integrated into a circuit that performs
energy harvesting, biosensing and wireless telemetry using a power-to-frequency
conversion scheme utilizing magnetic human body communication.
The unique battery-free operation is made possible by the team's
glucose biofuel cell (BFC) for obtaining power during operation while
simultaneously measuring changing glucose concentrations. Its energy-efficient
magnetic human body communication (mHBC) scheme operates in the 40-200 MHz
range to receive the time-resolved transmitted signals.
"It uses glucose present in the intestines as a biofuel to
power the device," said Mercier. "Making this all work with
ultra-low-power electronics and with a stable yet small glucose biofuel cell
were major technical challenges that were addressed here."
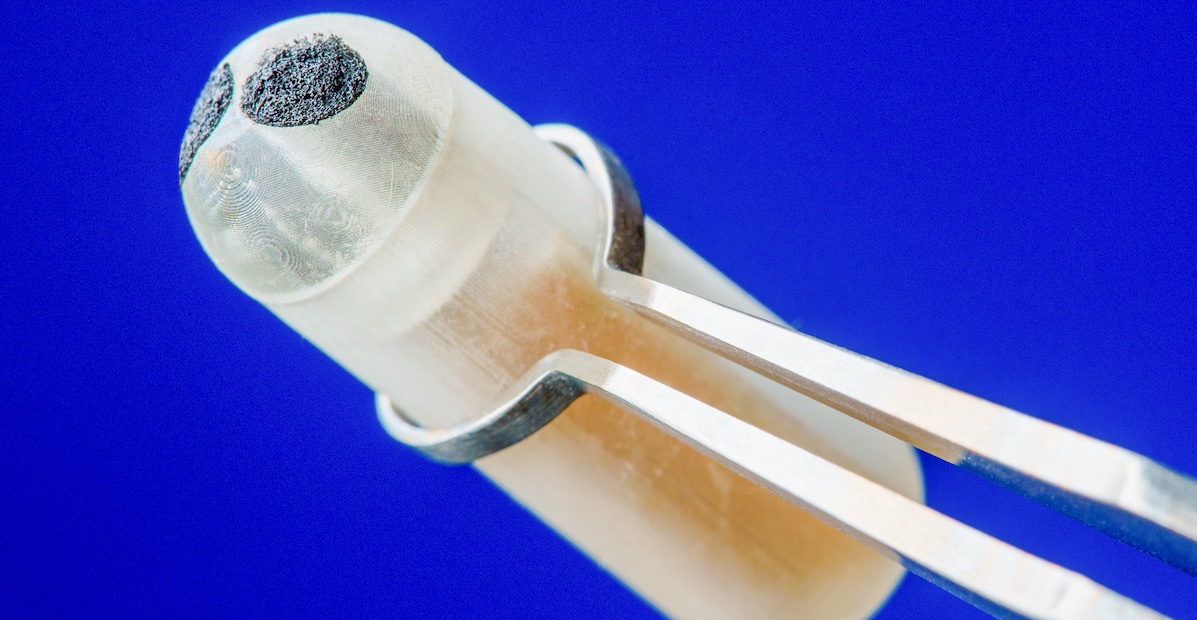
The proof-of-concept smart pill measures 2.6 cm in length and
0.9 cm in diameter. So far, small intestine data recording has only been
performed in pigs, which have a similar size GI tract to humans.
Next steps
Having achieved promising results in these experiments, the
researchers now plan to increase the number of sensors available in the pills.
This will enable monitoring of still more chemical parameters in the
intestines. They also plan to further miniaturize the sensors and electronic
circuitry to match what is currently available in the smart-pill market.
"Given that the gastrointestinal tract possesses dynamic
changes of pH, temperature and oxygen concentrations, future work envisions the
integration of additional sensing modalities to account for these
differences," said De La Paz Andres.
This project is a UC San Diego cross-campus collaboration
involving researchers from Department of Electrical and Computer Engineering,
and the Department of Nanoengineering at the UC San Diego Jacobs School of
Engineering; the UC San Diego Center for Wearable Sensors; the UC San Diego
Center for Microbiome Innovation; the Division of Gastroenterology at UC San
Diego Health; and the VA San Diego Healthcare System.
Along with De La Paz, Mercier and Wang, the research was
coauthored by Nikhil Harsha Maganti, Department of Electrical and Computer
Engineering, UC San Diego; Alexander Trifonov, Itthipon Jeerapan, Kuldeep
Mahato, Lu Yin, Thitaporn Sonsa-ard, Nicolas Ma and Won Jung, Department of
Nanoengineering, UC San Diego; Ryan Burns, Department of Electrical and
Computer Engineering, UC San Diego; and Amir Zarrinpar, Division of
Gastroenterology and Center for Microbiome Innovation, UC San Diego and VA San
Diego Healthcare System.
This research was supported by the UC San Diego Center for Wearable Sensors (CWS).