Not just safe and effective, but also heart-healthy
By THE MOUNT SINAI HOSPITAL /
MOUNT SINAI SCHOOL OF MEDICINE
Researchers at the Icahn School of Medicine at Mount Sinai have analyzed extensive datasets in the United States and found that individuals who were vaccinated against COVID-19 had fewer cases of heart attacks, strokes, and other cardiovascular issues among people who had been infected with SARS-CoV-2, the virus responsible for COVID-19.
Analyzing the most extensive datasets in the United States, researchers from the Icahn School of Medicine at Mount Sinai have revealed that vaccination against COVID-19 is associated with fewer heart attacks, strokes, and other cardiovascular issues among people who were infected with SARS-CoV-2, the virus that causes COVID-19.
The research letter, “Impact of Vaccination on Major Adverse
Cardiovascular Events in Patients with COVID-19 Infection,” was published on
February 20 in the Journal of the American College
of Cardiology.
In addition, the research will be presented in a poster session in New Orleans, LA, at the American College of Cardiology’s 72nd Annual Scientific Session Together With World Heart Federation’s World Congress of Cardiology.
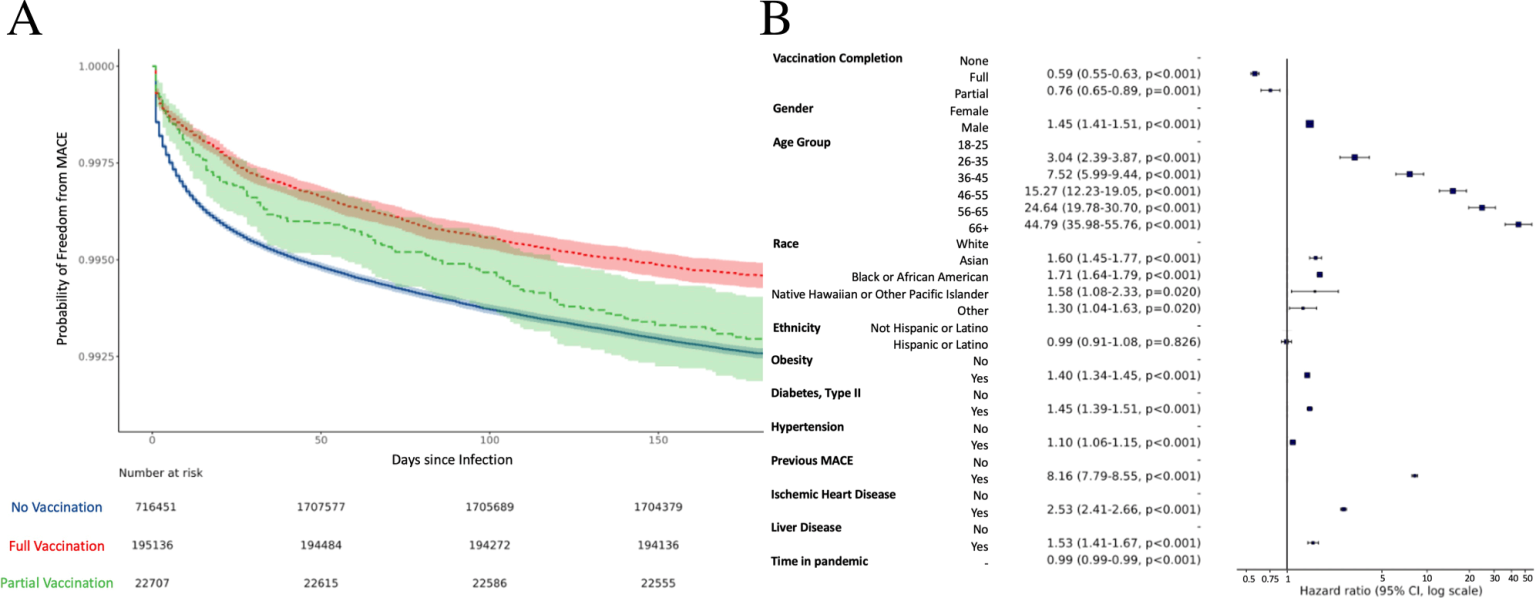
Figure A is a plot of the probability that patients do not develop MACE versus time since their initial SARS-CoV2 infection, stratified by vaccination status. Figure B is a depiction of hazard ratio associated with MACE according to each examined factor. For example, patients who were fully vaccinated were 59% as likely to achieve MACE compared to patients who were not vaccinated. Credit: Lab of Girish N. Nadkarni, MD, MPH, Icahn Mount Sinai
It is the first study to examine both full and partial vaccination and the link to major adverse cardiac events (MACE) in the United States, confirming similar analyses performed previously using the Korean COVID-19 registry.
Researchers used the National COVID Cohort Collaborative (N3C) database, the largest national comprehensive database on COVID-19. Since its inception in 2020, the N3C has continuously collected and harmonized data from electronic health records of institutions across the country.
Included in this study were
1,934,294 patients, 217,843 of whom received mRNA vaccine formulations by Pfizer-BioNTech
or Moderna or viral vector technology by Johnson & Johnson. Cox proportional hazards,
a statistical technique, was implemented to assess vaccination association with
MACE.
“We sought to clarify the impact of previous vaccination on
cardiovascular events among people who develop COVID-19 and found that,
particularly among those with comorbidities, such as previous MACE, type 2
diabetes, high cholesterol, liver disease, and obesity, there is an association
with a lower risk of complications. While we cannot attribute causality, it is
supportive evidence that vaccination may have beneficial effects on a variety
of post-COVID-19 complications,” said senior author Girish N. Nadkarni, MD,
MPH, Irene and Dr. Arthur M. Fishberg Professor of Medicine at Icahn Mount
Sinai, Director of The Charles Bronfman Institute of Personalized Medicine, and
System Chief, Division of Data Driven and Digital Medicine (D3M), Department of
Medicine.
“To our surprise, even partial vaccination was associated with
lower risk of adverse cardiovascular events,” said first study author Joy
Jiang, an MD/PhD candidate in the lab of Dr. Nadkarni. “Given the magnitude
of SARS-CoV-2 infection worldwide, we hope our findings
could help improve vaccination rates, especially in individuals with coexisting
conditions.”
Further work will be necessary to elucidate the mechanisms
involved from an immunological perspective and clarify the role of SARS-CoV-2
subtypes and reinfections in their relationship to the risk of MACE.
Reference: “Impact of Vaccination on Major Adverse Cardiovascular
Events in Patients With COVID-19 Infection” by Joy Jiang, Lili Chan, Justin
Kauffman, Jagat Narula, Alexander W. Charney, Wonsuk Oh, GIrish Nadkarni and on
behalf of the N3C Consortium, 10 February 2023, Journal
of the American College of Cardiology.
DOI:
10.1016/j.jacc.2022.12.006
Additional co-authors are Lili Chan, MD, MS; Justin Kauffman, BS;
Jagat Narula, MD, PhD; Alexander W. Charney, MD, PhD; and Wonsuk Oh, PhD, all
from Icahn Mount Sinai.
The work was supported, in part, by funds from the National
Institute of Diabetes and Digestive and Kidney Diseases of the National
Institutes of Health, grant numbers K23DK124645 and T32DK007757, and by the TL1
Career Development Award, 1TL1TR004420-01.
.webp)