Low risk, high effectiveness according to Brown researchers
Brown University
While mRNA vaccines against COVID-19 have been found to be safe and effective for the general population, in-depth evidence about safety and effectiveness for older adults and individuals with chronic health conditions is more limited.
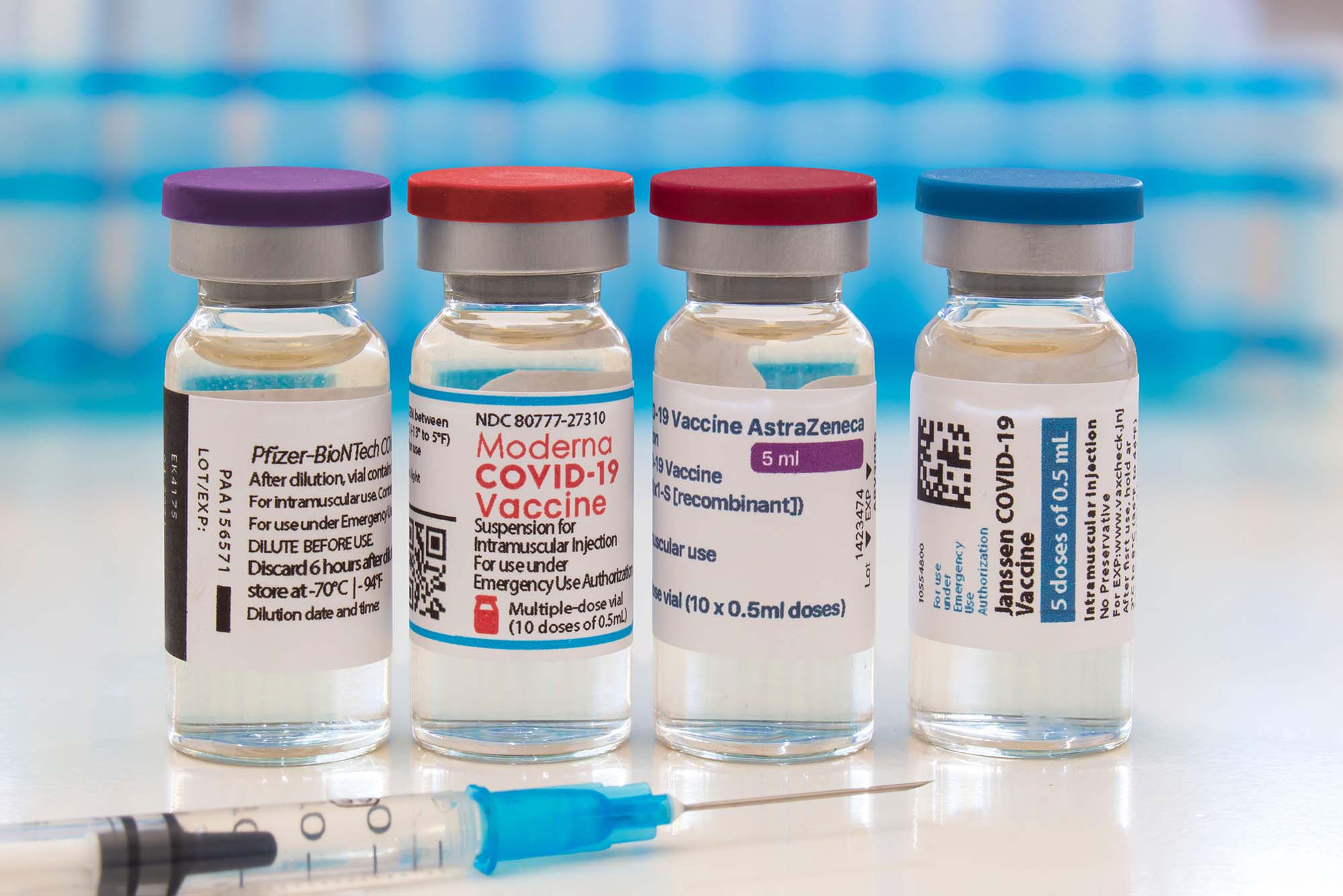
To address that gap, a team led by Brown
University researchers conducted the largest head-to-head comparison study of
the two mRNA vaccines approved by the U.S. Food and Drug Administration — the
Moderna and Pfizer-BioNTech vaccines. The results, published in JAMA Network Open,
showed that for older adults, the Moderna vaccine was associated with a
slightly lower risk of adverse events than the Pfizer-BioNTech vaccine.
“The results of this study can help public health experts weigh which mRNA vaccine might be preferred for older adults and older subgroups, such as those with increased frailty,” said lead study author Daniel Harris, an epidemiologist and research scientist in the Center for Gerontology and Healthcare Research at the Brown University School of Public Health.
The study looked at more than six million
older adults, with the average age of 76 years, who were vaccinated against
COVID-19 using one of the two mRNA vaccines, Moderna and Pfizer-BioNTech. The
vaccines have subtle differences in manufacturing, administration and immune
response.
The study confirmed that for older adults
in both vaccine groups, the risk of serious adverse events was very low. The
researchers also observed that for these older adults, the Moderna vaccine was
associated with a 4% lower risk of pulmonary embolism, which is a sudden
blockage in blood vessels of the lungs, and a 2% lower risk of thromboembolic
events, defined as several conditions related to blood clotting.
The Moderna vaccine was also associated
with a 15% lower risk of diagnosed COVID-19 compared to the Pfizer-BioNTech
vaccine.
Harris emphasized that the risk of adverse
events from a natural infection with SARS-CoV-2, the virus that causes
COVID-19, is substantially higher than the risk of adverse events from either
mRNA vaccine. But now that over 70% of the global population has received one
type of COVID-19 vaccine and vaccine supply is less of a concern, he said there
is a need for detailed information about vaccine effects and safety to guide
decision-making.
“Immunization with either mRNA vaccine is
substantially better and safer than not being vaccinated at all,” Harris said.
“But in an ideal world where we can have a choice between which vaccine product
is used, we wanted to see whether one vaccine was associated with better
performance for older adults and those with increased frailty.”
Harris said there is also a need to understand vaccine performance in real-world populations. He noted that older adults, who often have chronic health conditions, tend to be excluded from clinical trials or represented in small numbers. This is especially important considering that older adults, especially those in nursing homes, had a higher risk of developing severe COVID-19.
Older adults with frailty can also have
differences in their immune responses to vaccines, Harris said, making it
important to understand how these vaccines work for frail older adults compared
to their non-frail counterparts.
This research was part of a project called
the IMPACT Collaboratory, led by researchers at
Brown University and Boston-based Hebrew SeniorLife, which is enabling massive
monitoring of the long-term safety and effectiveness of COVID-19 vaccines for
Medicare beneficiaries, in collaboration with CVS and Walgreens pharmacies.
“Because we had these real-world data and a
cohort that included millions of older adults, we were able to tease apart
potentially very small differences in vaccine safety and effectiveness and
perform analyses on important clinical subgroups,” Harris said.
According to the research team, the improved
safety of the Moderna vaccine for some adverse events, like pulmonary embolism,
could have been due to its greater protection against COVID-19, especially for
non-frail older adults.
“We think that these two things, safety and
effectiveness, are interrelated,” Harris said. “The slightly reduced risk of
pulmonary embolism and other adverse events that we saw in individuals who
received Moderna may be because the Moderna vaccine was also more effective at
reducing COVID-19 risk.”
However, the study was unable to
definitively conclude whether the differences in adverse events were due to
safety or effectiveness, and the researchers recommended additional research in
this area. The study also only looked at the first dose of the mRNA vaccines,
so another potential next step could involve similar comparisons for subsequent
vaccinations.
“You can imagine regularly updating these
types of analyses as new vaccines are developed,” Harris said. “Depending on
which one comes out on top, even on a very small scale, that may have big
implications at the population level and render a preference for that
particular vaccine.”
Additional Brown University collaborators
included Kaley Hayes, Andrew R. Zullo, Vincent Mor, Preeti Chachlani, Yalin
Deng and Stefan Gravenstein.
The work was supported by the National
Institute on Aging of the National Institutes of Health under award number
U54AG063546, which funds NIA Imbedded Pragmatic Alzheimer’s Disease and
AD-Related Dementias Clinical Trials Collaboratory (the NIA IMPACT
Collaboratory). Supplemental funding was provided under grant numbers
4193U54AG063546-S07 and 3U54AG063546-S08.