Ah, maybe get vaccinated?
By OSAKA UNIVERSITY
It might start simply, with a cough or sneeze…but in some cases, the flu virus can make its way to your brain, causing serious symptoms or even death through a disease known as influenza-associated encephalopathy (IAE).
Now, in a study published in Acta Neuropathologica, researchers have revealed that
IAE may be caused by the virus entering the brain through a specific cell type,
and have identified possible treatment strategies.
Although IAE is increasingly common, surprisingly little
is known about how the influenza virus actually gets into the brain and causes
symptoms of encephalopathy (a general term for brain disorders). Notably, a
definitive treatment for IAE remains lacking, something that researchers from
Osaka University wanted to address.
To study how influenza viruses might cause IAE, the
research team used a range of methods. As well as looking for virus particles
in the brains of people who died from IAE, they created a mouse model of the
disease by injecting influenza A virus into the blood. They also used cell
culture methods to look at how well the virus infects different cell types.
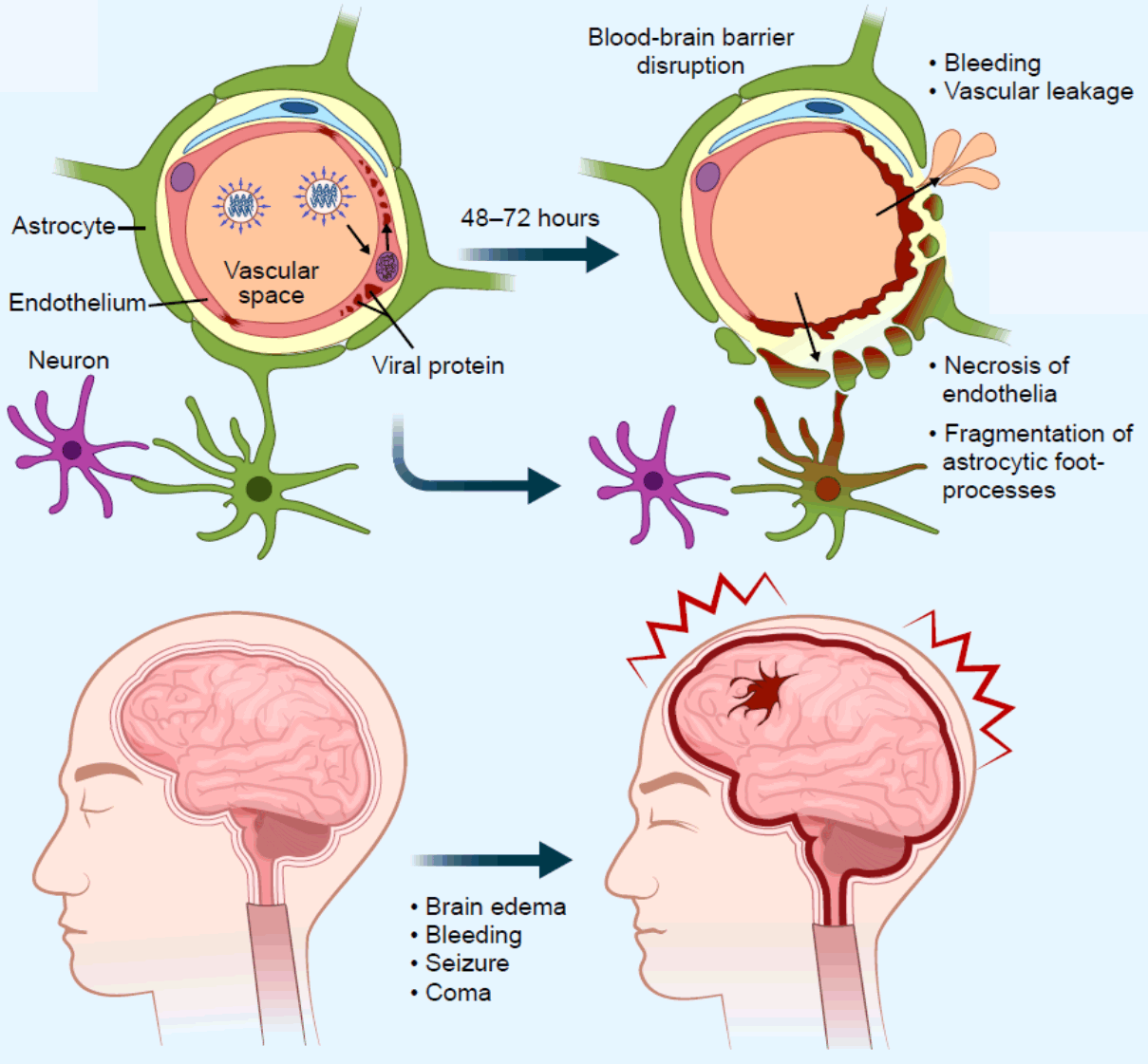
“In the human brains, the virus-injected mice, and the cultured cells, the influenza virus tended to accumulate in endothelial cells,” explains lead author of the study Shihoko Kimura-Ohba. “These cells create a barrier between the blood and the brain, and are important for protecting the brain from harmful substances.”
Accordingly, in both the human brains and the mouse
model, the barrier between the blood and the brain was compromised.
Furthermore, the researchers noticed that the virus wasn’t actually reproducing
within these endothelial cells—but there were a lot of proteins made by the
virus.
“When we saw this viral protein accumulation in the
brain, we realized that antiviral medications aimed at stopping viral
proliferation were unlikely to help,” says Tomonori Kimura, senior author of
the study. “However, antivirals aimed at stopping viral transcription and
translation—vital processes for making proteins—are also available.”
When the team tried these classes of antivirals in
endothelial cells treated with influenza virus, they observed less viral
proteins and cell death. In the mouse model of IAE, these antivirals were also
very effective when used early enough, suggesting that they may be useful in
human patients.
Given that many different kinds of viruses,
including COVID-19, can cause encephalopathy, these findings have
wide-ranging impacts. Moreover, although IAE care is improving, more than half
of all patients die or have long-lasting symptoms. A better understanding of
how viruses can cause encephalopathy will be important for developing new,
effective treatments.
Reference: “Viral entry and translation in brain
endothelia provoke influenza-associated encephalopathy” by Shihoko Kimura-Ohba,
Mieko Kitamura, Yusuke Tsukamoto, Shigetoyo Kogaki, Shinsuke Sakai, Hiroaki
Fushimi, Keiko Matsuoka, Makoto Takeuchi, Kyoko Itoh, Keiji Ueda and Tomonori
Kimura, 30 April 2024, Acta Neuropathologica.
DOI: 10.1007/s00401-024-02723-z