Bariatric surgery seems to be the winner
By AMERICAN SOCIETY FOR METABOLIC
AND BARIATRIC SURGERY
Systematic reviews of medical literature from 2020 to 2024 indicate that bariatric surgery, also referred to as metabolic or weight-loss surgery, results in the most significant and enduring weight loss compared to treatments with GLP-1 receptor agonists and lifestyle changes. These findings were presented at the 2024 Annual Scientific Meeting of the American Society for Metabolic and Bariatric Surgery (ASMBS).
Researchers found lifestyle interventions such as diet
and exercise resulted in an average weight loss of 7.4% but that weight was
generally regained within 4.1 years. GLP-1s and metabolic and bariatric surgery
proved far superior. Studies included thousands of patients from clinical
studies and several randomized clinical trials.
Five months of weekly injections of GLP-1 semaglutide
resulted in 10.6% weight loss and nine months of tirzepatide produced 21.1%
weight loss. However, once treatment stopped, about half the lost weight
returned within a year despite which drug was used. If injections were
continued, tirzepatide patients plateaued at 22.5% weight loss at 17-18 months.
Patients on semaglutide plateaued at 14.9% during the same time period.
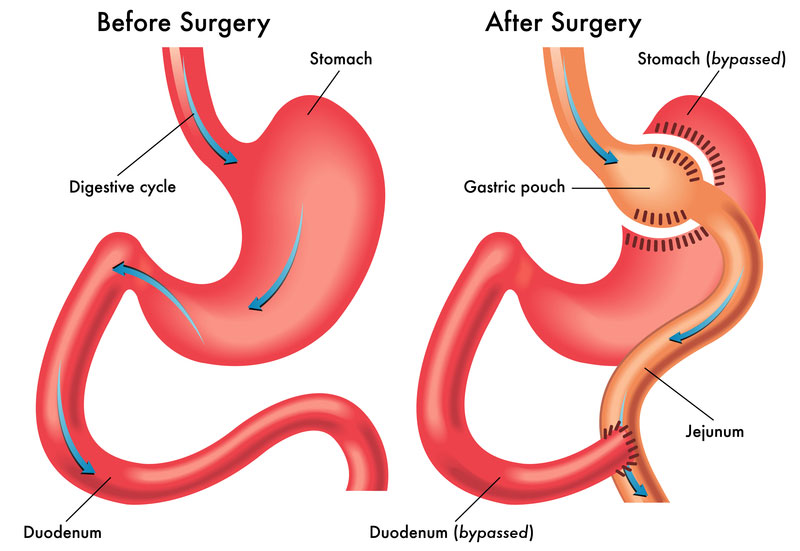
Metabolic and bariatric surgery procedures gastric bypass
and sleeve gastrectomy demonstrated total weight loss of 31.9% and 29.5% one
year after surgery, respectively. Weight loss of approximately 25% was
maintained for up to 10 years after surgery.
“Metabolic and bariatric surgery remains the most effective and durable treatment for severe obesity. Unfortunately, it also remains among the most underutilized,” said study co-author and bariatric surgeon Marina Kurian MD, NYU Langone Health. “Surgery needs to play a bigger role in obesity treatment and be considered earlier in the disease process. It is no longer a treatment of last resort and should not be withheld until more severe disease develops. There is no medical reason for this.”
The ASMBS reports that in 2022 nearly 280,000
metabolic and bariatric procedures were performed in the U.S., which represents
only about 1% of those who meet eligibility requirements based on BMI.
According to the U.S. Centers for Disease Control and Prevention (CDC), obesity
affects 42.4% of Americans. Studies show the disease can weaken or impair the
body’s immune system and cause chronic inflammation and increase the risk of
many other diseases and conditions including cardiovascular disease,
stroke, type 2 diabetes, and certain cancers.
“While the new drug treatments show great promise and
will lead to more people being successfully treated, particularly if prices
come down and insurance coverage improves, we are barely using the best tool we
have to fight obesity — metabolic and bariatric surgery, which is safer and
more effective than ever before,” said Ann Rogers, MD, ASMBS President-elect
and Professor of Surgery at Penn State College of Medicine, who was not
involved in the study. “For many people, the risk of death from obesity, diabetes,
and heart disease exceeds the risks of surgery.”
Study Methodology
The study included a systematic review of studies that
examined weight loss through lifestyle modification, GLP-1s (Semaglutide or
tirzepatide), or metabolic and bariatric surgery. GLP-1 data included four
randomized clinical trials conducted between 2021 and 2024 while conclusions on
lifestyle modifications were based on a systematic review of eight studies.
Metabolic and bariatric surgery (gastric bypass and sleeve gastrectomy) were
subject to a review of 35 studies, including two randomized clinical trials. In
all, researchers reviewed the weight-loss results of approximately 20,000
patients.
Reference: “Effectiveness and Durability of Common Weight Loss Methods”
by Megan E Jenkins, Juliane Hafermann, Christine Fielding, Gerhard Prager and
Marina Kurian, 11 June 2024, American Society for Metabolic and Bariatric
Surgery (ASMBS) 2024 Annual Scientific Meeting.